
Beijing Hospital of Traditional Chinese Medicine Dermatology Department
Open, Share, Active, Win-Win
Every Wednesday
12:00
Follow Updates · Click the star in the upper right cornerStar
See in Time · Click the lower right cornerLooking

Speaker Introduction

Xu Jun Tao, Master of Medicine, graduated from Chengdu University of Traditional Chinese Medicine, studied under Professor Tang Dingshu, and has followed renowned TCM dermatologists such as Professor Zhong Yize and Professor Ai Rudi to study TCM dermatology. He has also studied dermatology and venereology at West China Hospital of Sichuan University. After starting work, he was awarded the title of “Technical Expert of Zhengzhou City” and has furthered his studies at the Air Force General Hospital Dermatology Hospital. In 2019, he learned TCM surgery from Li Zhongyu, the inheritor of Zhang Bagua Surgery.
Specialty: Proficient in the combined treatment of acne, seborrheic dermatitis, seborrheic alopecia, eczema, chloasma, psoriasis, vitiligo, acute and chronic urticaria, flat warts, herpes zoster, and skin vasculitis using both TCM and Western medicine; skilled in dermatoscopy and has clinical experience in diagnosing difficult pigmentary skin diseases.


Lecture Content
Thank you for the introduction and the invitation from the teacher. Today, I would like to share some experiences in treating plaque psoriasis through voice. First, I would like to thank Director Zhang Cang for providing us with such a great academic platform, allowing us to learn new knowledge and different teachers’ experiences every week, which continuously improves our academic level. Thank you again, Teacher Zhang.
Respected directors, professors, teachers, and colleagues, good evening. I am Xu Jun Tao from the Dermatology Department of Henan Provincial Hospital of Traditional Chinese Medicine. Today, I will discuss a medication and a method for treating plaque psoriasis. Let’s first review the Western medical treatment guidelines for plaque psoriasis. For mild plaque psoriasis, the first choice of topical medications includes four major categories: the first is potent corticosteroids, the second is vitamin D3 derivatives, the third is retinoids, and the fourth is coal tar preparations.
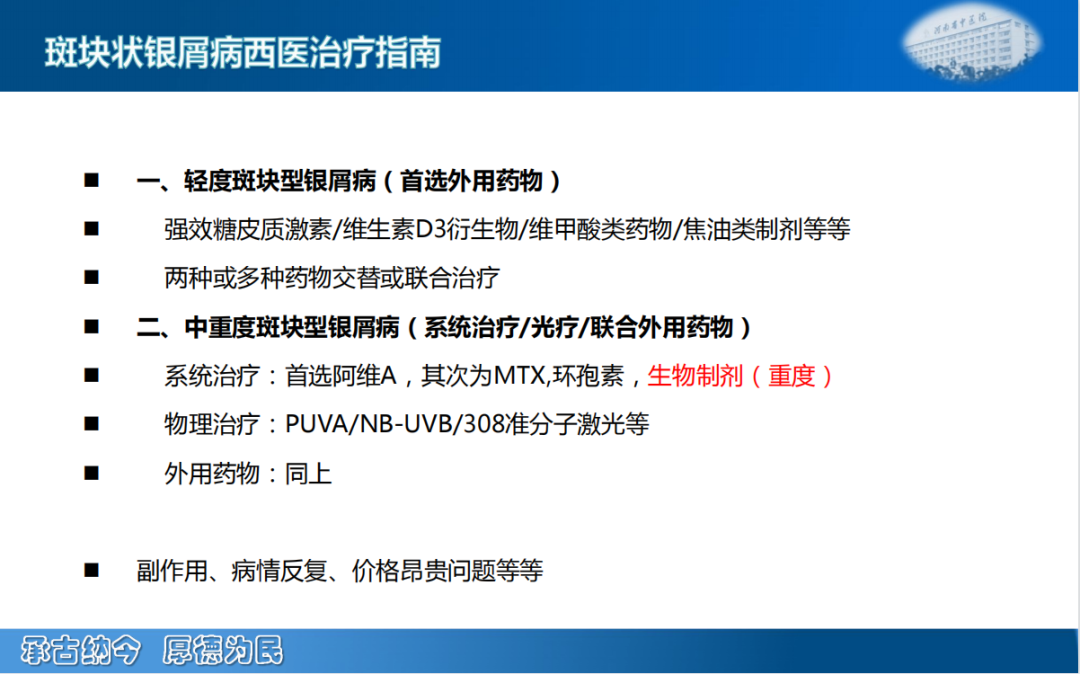
Potent corticosteroids mainly have strong anti-inflammatory effects. Commonly used ones include halobetasol ointment and clobetasol propionate ointment. Vitamin D3 derivatives mainly refer to calcipotriene ointment, while retinoids mainly refer to tretinoin. Coal tar preparations mainly refer to coal tar. These four types of medications have different effects. Potent corticosteroids have a strong anti-inflammatory effect and act quickly, but their side effect is that long-term use can lead to skin atrophy. The second is vitamin D3 derivatives, which we use more often, such as calcipotriene ointment. This medication acts slowly and is relatively expensive, but its side effects are relatively minor. The third category is retinoids, which can also act topically. They mainly regulate keratinocyte differentiation, but some people may find them irritating to the skin, causing redness, irritation, and itching, and some may develop irritant dermatitis. The fourth category is coal tar preparations, which are used less frequently in clinical practice due to their strong odor, making them less acceptable to some patients.
Currently, the medications we use most in clinical practice are combinations of two or more medications, such as the combination of potent corticosteroids and vitamin D3 derivatives, for example, calcipotriene and betamethasone ointment, and the combination of potent corticosteroids and retinoids, such as compound clobetasol propionate ointment. These combinations can achieve good therapeutic effects while reducing some side effects of the medications, so they are commonly used in clinical practice. Of course, the price of these combined preparations is also relatively high.
For moderate to severe plaque psoriasis, we generally advocate systemic treatment, along with enhanced physical therapy and topical preparations. The first choice of systemic medication is acitretin, which has relatively few side effects, the most significant being elevated blood lipids. Some people may experience dry mouth and mucosal dryness after use, and it is contraindicated for women of childbearing age; if taken, contraception must be practiced for at least three years.
The second medication is methotrexate and cyclosporine, which are immunosuppressants. Regular liver function tests are required to monitor the side effects of these medications.
Currently, biologics are quite popular and have good efficacy for moderate to severe plaque psoriasis, targeting interleukin-23, interleukin-17A, and tumor necrosis factor. These medications are used frequently in clinical practice and act quickly, but they are relatively expensive.
Another physical therapy we commonly use is narrowband UVB and 308 nm excimer laser. For smaller areas, the 308 nm excimer laser is quite effective, typically administered once or twice a week. Narrowband UVB is generally administered every other day, three times a week, and is also effective, but some people may experience overall skin darkening after treatment, which is a concern for those who are particularly beauty-conscious.
For topical medications, as mentioned earlier, the same medications used for mild plaque psoriasis are also used for moderate to severe plaque psoriasis.
In summary, the Western medical treatment for plaque psoriasis involves topical medications combined with systemic treatment and physical therapy. However, due to the significant side effects of corticosteroids and vitamin D3 derivatives, or their high costs, it can be challenging to achieve an optimal treatment outcome in clinical practice. Today, I would like to share my method for treating plaque psoriasis—using traditional Chinese medicine combined with cupping therapy.
First, let’s discuss the use of Wudai Ointment for treating plaque psoriasis. Before that, I would like to share a case.
Ding, male, 23 years old, a student at a university in Zhengzhou. He was hospitalized for treatment on January 15, 2013. Chief complaint: recurrent erythema and scales all over the body with itching for 8 years, worsening for half a year. Medical history: 8 years ago, without obvious cause, erythema and scales appeared on the scalp, which gradually spread all over the body. He had previously received treatment at clinics and dermatology outpatient departments, taking both Chinese and Western medicines, but with poor efficacy. Half a year ago, the skin lesions worsened, with erythema and scales spreading on the scalp, trunk, and limbs, presenting in patches, with no deformities in the joints.
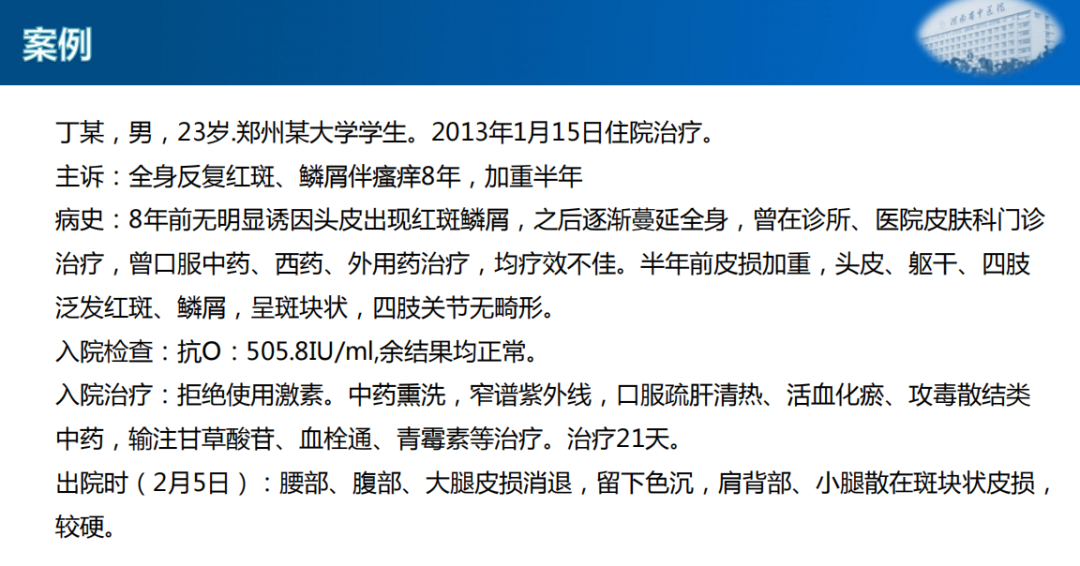
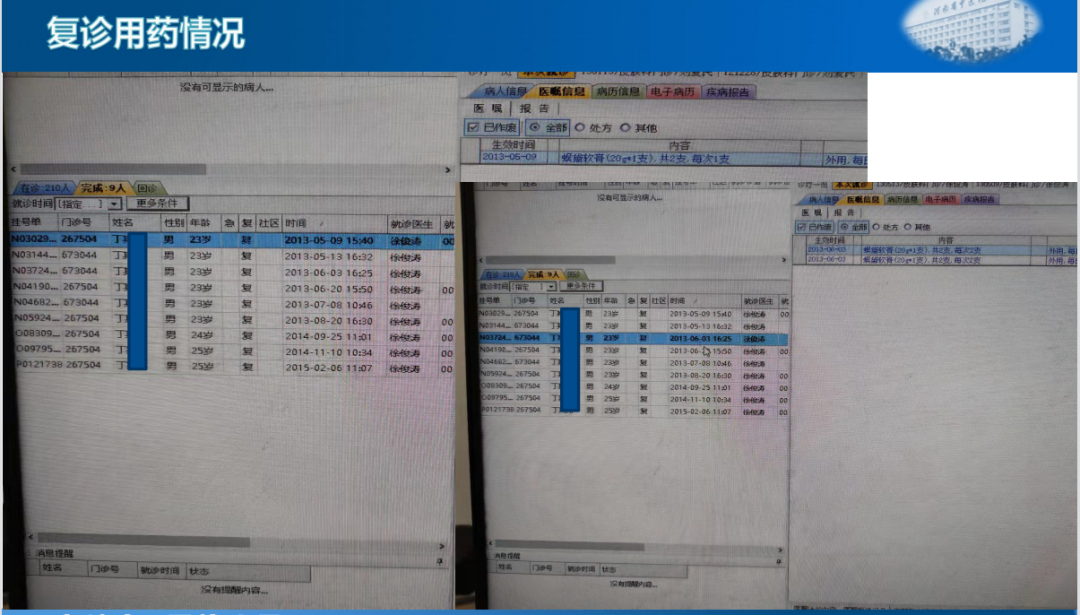
I remember this patient clearly; he was hospitalized in January because he wanted to quickly alleviate his skin lesions before his graduate school entrance exam in February. After admission, a series of tests were conducted, including blood routine and liver and kidney function tests, all of which were normal. However, the anti-streptolysin O titer was relatively high, over 500, while the other results were normal. Since the patient refused to use corticosteroids, we used traditional Chinese medicine for fumigation treatment, along with narrowband UVB therapy, and administered a Chinese herbal formula to soothe the liver, clear heat, invigorate blood circulation, and dispel toxins, along with infusions of glycyrrhizin, thrombolytic agents, and penicillin. After about 21 days of treatment, the patient was discharged on February 5, with the skin lesions on the waist, abdomen, and thighs regressing, leaving behind some pigmentation. The lesions on the shoulder and calf were still present and relatively hard, and various methods were tried to alleviate them, but they did not easily regress, so the patient was discharged. After discharge, he was busy with his entrance exam and did not return for follow-up. In May, he came back with some scattered recurrences of skin lesions. As a student, he did not have the funds for long-term treatment and expressed a desire to use topical Chinese patent medicine instead of traditional Chinese medicine, which he found too time-consuming. I suggested he try Wudai Ointment, which had just arrived at our hospital. He had previously used Binghuangfule Ointment with unsatisfactory results, so I recommended he try Wudai Ointment. The patient was compliant, and since the instructions for Wudai Ointment indicated it was primarily for chronic eczema and chronic dermatitis, he agreed to try it. On May 9, we prescribed him 2 tubes of Wudai Ointment, and by May 13, after using it for 4 days, he returned to report, “Doctor Xu, this is quite effective; my newly developed skin lesions have regressed, and the previously thick lesions have also flattened significantly.” I was surprised by the effectiveness, and later on May 13, I prescribed him 4 more tubes for external use.
After using the ointment, the results exceeded my expectations; sometimes it was even more effective than Western medicine. The patient returned twice in May and June, and after August, he did not come back, indicating that his condition was likely well controlled. In September 2014, exactly one year later, he returned with a slight recurrence. He said, “Doctor Xu, please prescribe me Wudai Ointment again.” I prescribed him a few tubes to take home. After using it, his condition was well controlled, and he did not have any recurrences for over a year. On February 6, 2015, he came back to request Wudai Ointment again, but after that, he did not return for unknown reasons, possibly because he had recovered or for other reasons.
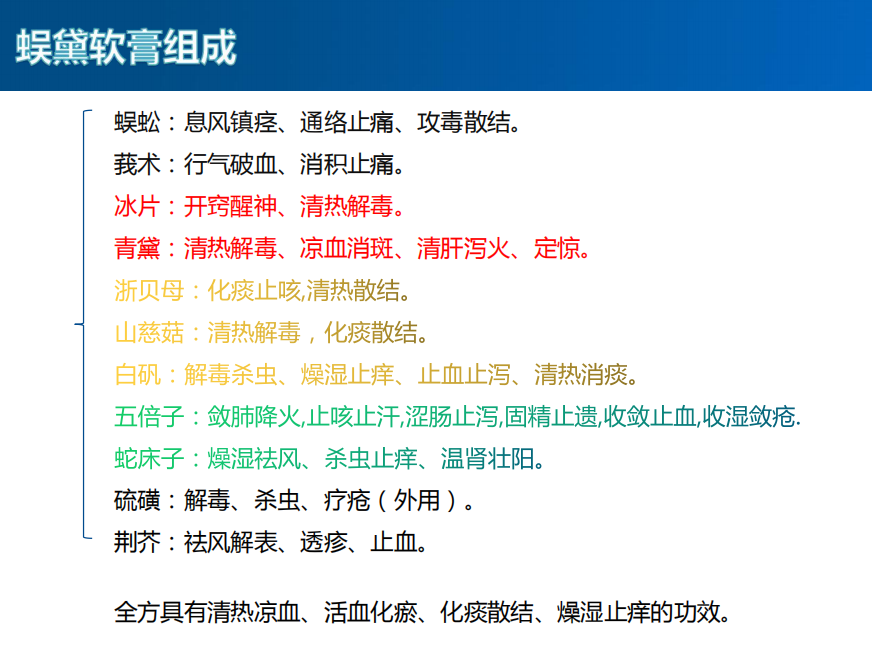
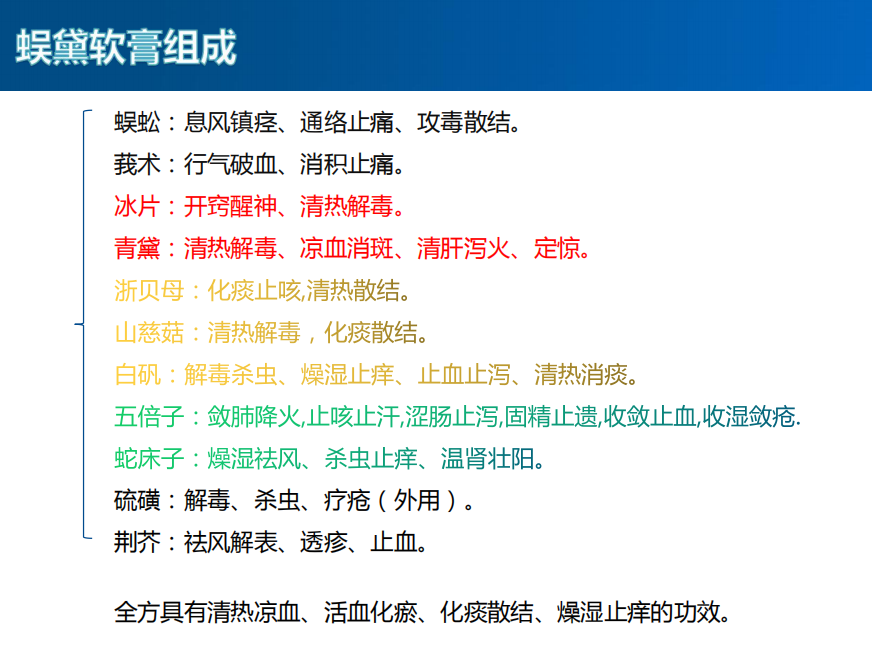
In summary, Wudai Ointment has shown good efficacy for this condition. Due to its effectiveness, I became interested in its composition, which includes centipede (wugong), cnidium (shechuangzi), sulfur (liuhuang), alum (bai fan), Zhejiang fritillary (zhebeimu), indigo (qingdai), phellodendron (huangbo), mountain yam (shancigu), galla chinensis (wubeizi), borneol (bingpian), schizonepeta (jingjie), and curcuma (ezhu). The ointment is a brownish-gray-green paste with a borneol fragrance, and its main functions are to clear heat, dry dampness, dispel wind, and relieve itching. It is primarily used as an adjunct treatment for subacute and chronic eczema caused by wind-heat, although its instructions do not mention psoriasis.
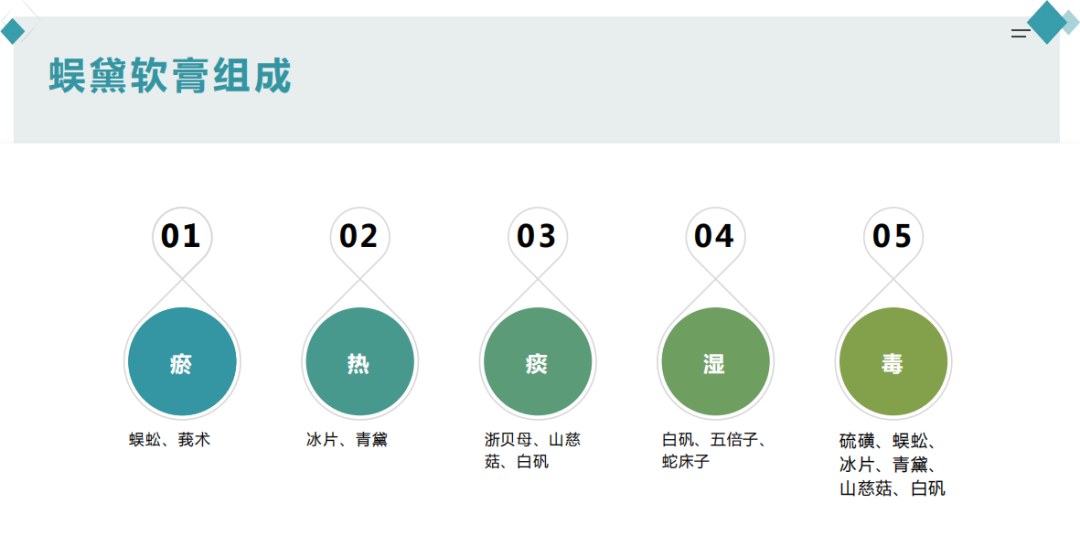
I reviewed some literature, and it was reported that this ointment is effective for chronic eczema, dermatitis, nodular scabies, pityriasis rosea, herpes zoster, and roseola. However, there was no mention of its efficacy for psoriasis. I then summarized the herbal composition of the ointment: centipede and curcuma are mainly blood-activating and stasis-dispelling herbs; borneol and indigo are primarily blood-cooling, heat-clearing, and detoxifying herbs; Zhejiang fritillary, mountain yam, and alum mainly have phlegm-resolving and stasis-dispelling effects. Galla chinensis and cnidium are primarily damp-drying and moisture-removing herbs, while sulfur is used for killing parasites and relieving itching. Schizonepeta is used for dispelling wind and relieving itching. The combination of these herbs results in a formula that clears heat, cools blood, invigorates blood circulation, and resolves phlegm and stasis. Further summarizing, the overall efficacy of Wudai Ointment targets stasis, heat, phlegm, dampness, and toxins.
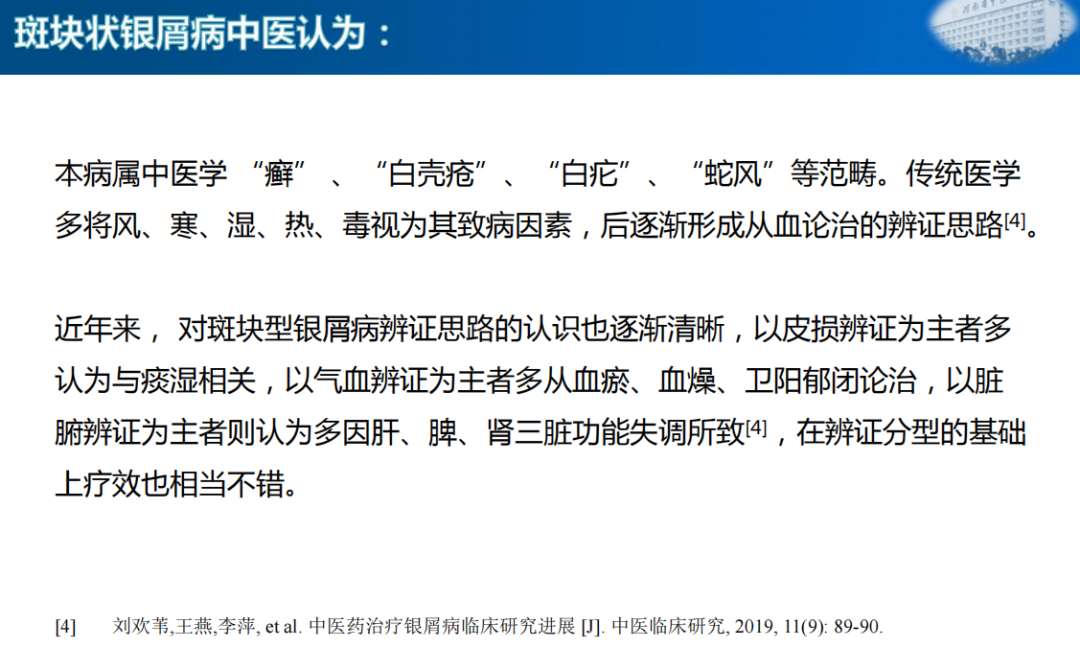
Having discussed Wudai Ointment, let’s briefly analyze the TCM causes of plaque psoriasis. I reviewed some literature, and TCM considers this condition to fall under the categories of tinea, white shell sore, and white scab, referred to as “shefeng”. Traditional medicine often views wind, cold, dampness, heat, and toxins as pathogenic factors, gradually forming a treatment approach based on blood theory. In recent years, the understanding of the syndrome differentiation for plaque psoriasis has become clearer, with those focusing on skin lesions often associating it with phlegm-dampness, while those focusing on qi and blood differentiation often consider it related to blood stasis, blood dryness, and obstruction of defensive yang. Those focusing on organ differentiation often attribute it to dysfunction of the liver, spleen, and kidneys. Based on these differentiation types, effective treatments have been achieved.
Those focusing on skin lesions, represented by An Lihui, believe that long-standing blood stasis transforms into phlegm, which further affects the circulation of qi and blood, leading to phlegm and stasis obstructing the skin, hence the clinical manifestations of dark red patches and a dark red tongue. Clinical treatment that invigorates blood circulation and dispels stasis while supplementing phlegm-resolving herbs has achieved ideal results. Therefore, he believes that phlegm and stasis are the causes of plaque psoriasis.
Those focusing on qi and blood differentiation, represented by Professor Zhuang Guokang, believe that stasis heat obstructs the blood vessels, which is the main pathogenesis of plaque psoriasis. Based on differentiation, using blood-invigorating methods has achieved satisfactory results. He believes that plaque psoriasis is caused by blood stasis.
Those focusing on organ differentiation, represented by Professor Ma Shaoyao, believe that the occurrence of psoriasis is determined by the physiological functions of the liver in regulating and storing blood, as well as the pathological interactions between the liver and other organs. He proposed nine methods for treating psoriasis based on liver differentiation, using liver-soothing and qi-invigorating methods to dispel stasis, achieving ideal results. In summary, the causes of plaque psoriasis are often attributed to the mutual obstruction of phlegm, heat, and stasis, and the treatment with Wudai Ointment directly addresses diseases caused by phlegm, heat, stasis, and toxins. Therefore, according to the TCM principle of treating different diseases with the same method, Wudai Ointment can be used externally for plaque psoriasis.
When I was invited to give a lecture at the gathering last month, I checked again to see if there were any clinical reports on Wudai Ointment for treating psoriasis. I found that indeed there are. In December of last year, Shang Shuqin from Hunan University of Traditional Chinese Medicine and Professor Xi Jianyuan from the First Affiliated Hospital of Hunan University of Traditional Chinese Medicine published an article in the Journal of Guangxi University of Traditional Chinese Medicine. Their article titled “Clinical Observation of Wudai Ointment in the Treatment of Plaque Psoriasis in the Stationary Phase” involved 70 patients with stationary plaque psoriasis, randomly divided into two groups of 35 each. The control group was treated with calcipotriene ointment, while the observation group was treated with Wudai Ointment for a duration of 6 weeks. They observed that the treatment efficiency in the observation group was 94.29%, while the control group was 77.14%. The PASI score for the severity of psoriasis lesions and the quality of life survey indicated that the observation group had better efficacy than those treated solely with calcipotriene ointment, further confirming the viewpoint that Wudai Ointment can treat plaque psoriasis.
In the second part, I will discuss cupping therapy for treating plaque psoriasis. In recent years, with national policy guidance, various hospitals have advocated the use of traditional Chinese medicine and therapies to treat skin diseases. Many people have used cupping therapy for treating plaque psoriasis and other skin diseases, achieving good results. I will not go into the specifics of how to perform it, but I will briefly share some of its mechanisms of action.
Cupping therapy was first mentioned in the “Fifty-Two Disease Formulas” as a method that uses suction and combustion to create negative pressure within the cup, which is then applied to the treatment area. Cupping therapy is a special technique of cupping, also known as quick cupping or kissing cupping. It involves repeatedly applying and immediately removing the cup from a specific area of the body, which has the effects of warming, dispelling cold, and promoting blood circulation. It is commonly used to treat facial paralysis and has been widely applied in dermatology in recent years, often used for treating urticaria, acne, herpes zoster, and chloasma. Moving cupping is another special technique of cupping, also known as sliding cupping, which was previously used mainly for treating internal diseases. Due to its strong suction and deep action, along with the rapid movement of the cup on the skin, it can promote blood flow, soften hard masses, dispel stasis, and invigorate qi. This therapy is commonly used for treating musculoskeletal and connective tissue diseases, respiratory system, nervous system, digestive system, skin, and subcutaneous tissue diseases. When performing moving cupping, a medium is required, and the efficacy varies significantly depending on the medium used. Therefore, we cannot perform moving cupping directly on the skin, as it would be painful for the patient and difficult to execute due to the skin’s texture. We typically use mediums such as petroleum jelly, safflower oil, or homemade medicinal liquids. Regarding the medium, I have considered whether Wudai Ointment could be used as a medium for moving cupping.
Since Wudai Ointment has shown such good external efficacy, combined with moving cupping, it can not only provide lubrication to facilitate the cupping process but also exert its medicinal effects. Therefore, I wondered if Wudai Ointment could be used as a medium for moving cupping. After reviewing a large amount of literature, I found no reports of Wudai Ointment being used as a medium for moving cupping therapy. Based on my clinical experience, I chose Wudai Ointment as the subject of my research to observe the effects of Wudai Ointment combined with moving cupping in treating plaque psoriasis. (To be continued next Wednesday)
Welcome to Follow
This article is based on the audio recording of Xu Jun Tao’s lecture at the Dermatology Department of Beijing Hospital of Traditional Chinese Medicine, organized by volunteers. It was first published on the WeChat subscription account of the Zhao Bingnan TCM Dermatology School. Please indicate the speaker, organizer, and source when reprinting.
Organizer:
Wang Siqing, Beijing University of Traditional Chinese Medicine
Ma Huanwei, Tianjin Puri Hospital
Compiler:
Jiang Shufeng, Air Force Specialty Medical Center
Editor:
Xu Xiaojing, Changping Chengnan Center

Welcome to Like, Follow, and Share

