

Author: Keenman
After a family member is diagnosed with a tumor, one of the most important tasks for us as relatives is to navigate through different hospitals and oncology departments to inquire about treatment options. This is crucial whether we are determining the first-line treatment plan at the onset of the illness or seeking subsequent treatment options after resistance to the first-line therapy.
Due to the large number of cancer patients in the country, there is a severe shortage of oncologists, especially renowned cancer specialists. With the addition of emergency appointments, a doctor may face dozens of patients in a single morning, and the time allocated for each patient’s consultation is often less than 15 minutes. How to communicate effectively with the doctor within this limited consultation time is something we need to consider seriously.
When we post on forums to document the treatment process for our loved ones, it is a “one-on-one” service. Sometimes we assume that since we have seen the same doctor several times, they should remember our family member’s previous treatment records. However, the reality is that doctors face dozens of patients daily, accumulating thousands of patients over the year. It is challenging for doctors to accurately remember your family’s medical history and treatment process, even if you have been following the same doctor since the initial diagnosis, let alone if there have been changes in the attending physician.
The “Dancing with Cancer” forum regularly organizes Q&A sessions within the patient community. To ensure that the participating doctors can obtain the necessary information to provide treatment suggestions in a short time, I specifically asked Director Zhang Hongmei from Beijing Chest Hospital to compile the essential information based on her years of experience (using lung cancer patients as an example, including but not limited to the following information):
1. What is the pathological type and staging?
2. What are the specific conditions inside and outside the lungs, such as the location and size of lung lesions, whether they are multiple or single? What are the specific locations and morphological sizes of extra-pulmonary lesions?
3. Relevant hematological test results (including gene testing results, dynamic changes in tumor markers, etc.)
4. For non-first-line patients, what were the previous treatment plans and dosages? What was the efficacy after medication? (This should be specific to changes in lesions in various parts of the body).
5. How was the tolerance to chemotherapy?
6. Age, physical condition, and any underlying diseases?
7. It is best to bring imaging data (films), as the imagination brought by simple textual descriptions in imaging reports can be limited and restrict the doctor’s structural understanding of the images.
8. For patients who cannot attend consultations, especially during the pandemic, it is helpful to record a short video of the patient’s current condition.
And so on…
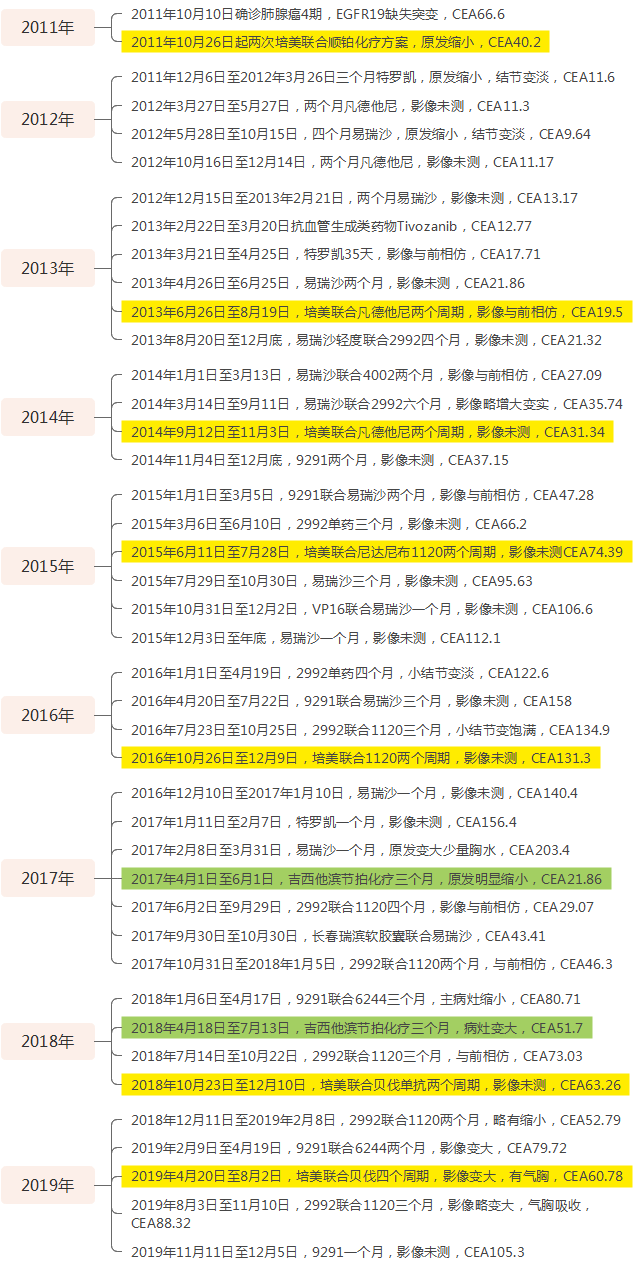
As a long-time companion in my mother’s battle against cancer, during critical treatment moments, I often consult many professional doctors and seek advice from experienced patients. Before consulting them, I carefully organize my mother’s treatment process according to the above requirements. Since my mother has been fighting cancer for nearly eleven years, the main treatment post on the forum contains over 16,000 words, printed out to nearly 30 pages, which takes a long time for anyone to read. Considering that doctors’ time is very precious, I specifically created a concise version of my mother’s treatment process, printed it out, and took it to the hospital for consultations so that doctors could quickly understand the medical history and treatment process.
As I previously wrote in “Crossing Ten Years – Dreams Create Miracles”, the most important thing in a long-term dance with cancer is to learn how to be a family member of the patient. Properly managing the relationship with doctors, the relationship between medical treatment and life, and the relationship between trusting doctors and self-learning is the starting point of the long journey of fighting cancer. As family members, we should spend more time and energy organizing information, which not only shows respect for the doctors but also allows us to save time in effective communication, enabling us to ask doctors about some cutting-edge treatment knowledge.
Below, I will use the consultation materials I prepared earlier this year after my mother developed resistance to nearly a year of Nivolumab (O drug) immunotherapy as an example to demonstrate to fellow patients how to prepare a concise consultation document.
Consultation Materials Prepared in January 2022

1. Patient: Female
2. Date of Birth: August 22, 1949
3. Physical Condition: Lives normally like an average person, no other underlying diseases;
4. Pathological Type: Lung adenocarcinoma, stage IV, no surgery or radiotherapy performed
5. Specific Conditions Inside and Outside the Lungs: Primary lesion in the right lower lung, multiple millet-like nodules in both lungs, lymph node metastasis, no bone metastasis, no brain metastasis;
6. Genetic Mutation Status:
(1) In November 2011, CT-guided biopsy for pathological testing revealed EGFR exon 19 deletion;
(2) In December 2016, blood sent for CTDNA testing only detected FGFR1 non-driver gene mutation (0.7%), no EGFR mutations detected;
(3) In November 2018, blood sent for CTDNA testing targeting EGFR fragments also did not detect any EGFR mutations;
(4) In November 2019, re-biopsy of the enlarged primary lesion for FoundationOne testing detected T790M mutation with an abundance of 0.0314, the original EGFR19 mutation abundance was 0.4614, with a ratio of EGFR19 mutation to T790M mutation of 14.7:1;
(5) On March 3, 2021, peripheral blood sent for ctDNA testing only showed the 19 mutation with an abundance of 0.31%;
(6) On December 26, 2021, again sent peripheral blood for ctDNA testing, still only the 19 mutation with an abundance of 0.38%;
7. Chemotherapy Tolerance: Previously used chemotherapy drugs include Pemetrexed combined with Cisplatin, Pemetrexed combined with Bevacizumab, and single-agent Gemcitabine, all of which were effective. Oral administration of Vinorelbine soft capsules and Etoposide soft capsules showed no significant effect. Single-agent chemotherapy tolerance is acceptable.
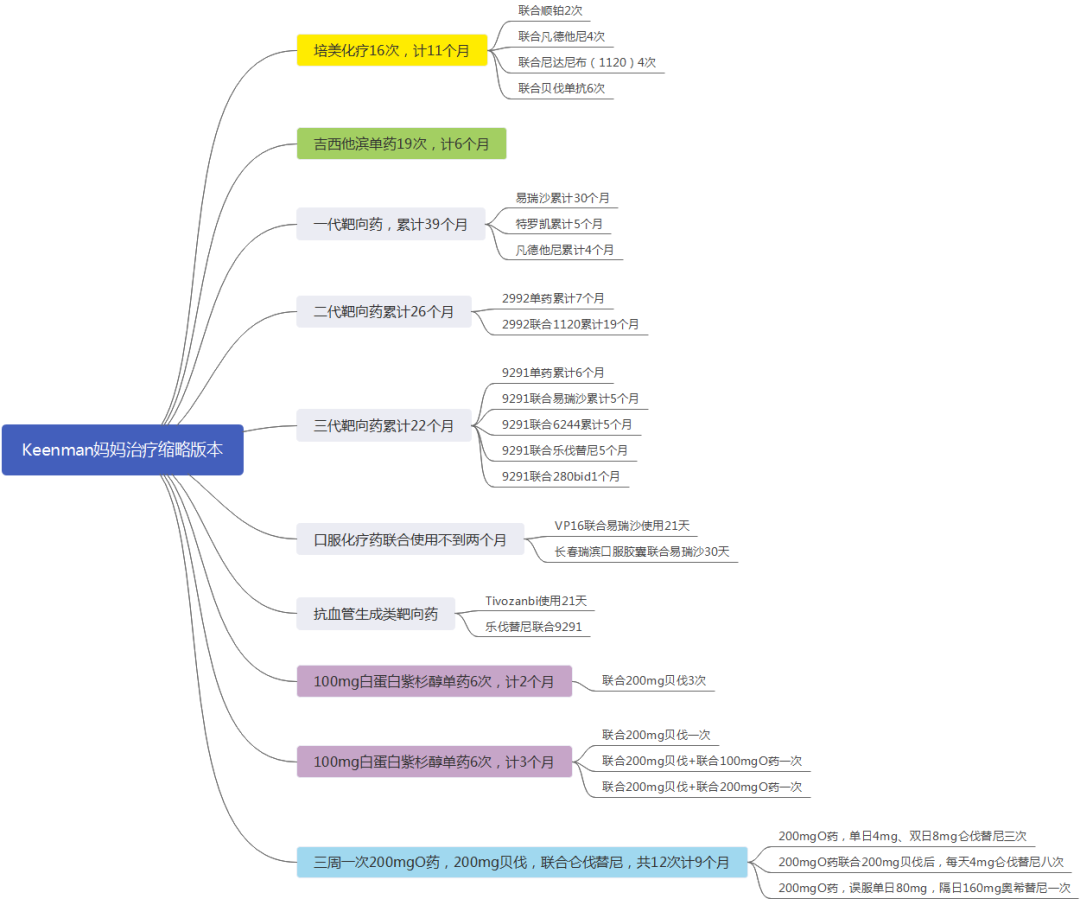
8. Brief Summary Version:
Mainly used targeted chemotherapy in a sequential interspersed manner, generally requiring two chemotherapy sessions each year, thus integrating and summarizing the targeted drugs and chemotherapy used.
(1) Pemetrexed chemotherapy 16 times, including 2 times combined with Cisplatin, 4 times combined with Vandetanib, 4 times combined with Nintedanib (BIBF1120), and 6 times combined with Bevacizumab, totaling 11 months, marked in yellow in the text;
(2) Gemcitabine single-agent reduced dosage for a three-week regimen on days 1, 8, and 15, 19 times, totaling 6 months, marked in green in the text;
(3) Albumin-bound Paclitaxel reduced dosage combined with Bevacizumab for a three-week regimen on days 1 and 8, 12 times, totaling 5 months, marked in purple in the text;
(4) Erlotinib used alone or as a main drug for a total of 30 months;
(5) Vandetanib used alone for 4 months;
(6) Afatinib (2992) used alone or as a main drug for a total of 26 months;
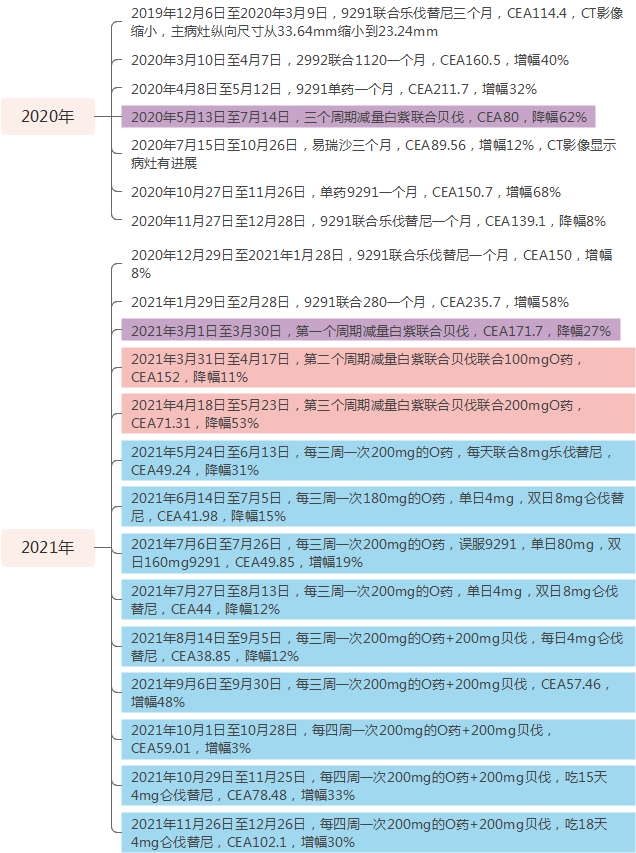
(7) Osimertinib (9291) used alone or as a main drug for a total of 22 months;
(8) Anti-angiogenic targeted drug Tivozanib AV851 used for about 1 month;
(9) From March 28, 2021, to December 26, 2021, a total of Nivolumab (O drug) immunotherapy was used, including 4 times every three weeks, then daily combined with 4mg every other day of Lenvatinib, and another 8 times with 200mg combined with 200mg of Bevacizumab, starting from the 8th day after each Bevacizumab infusion, using 4mg of Lenvatinib until the second immunotherapy cycle. The specifics are as follows:
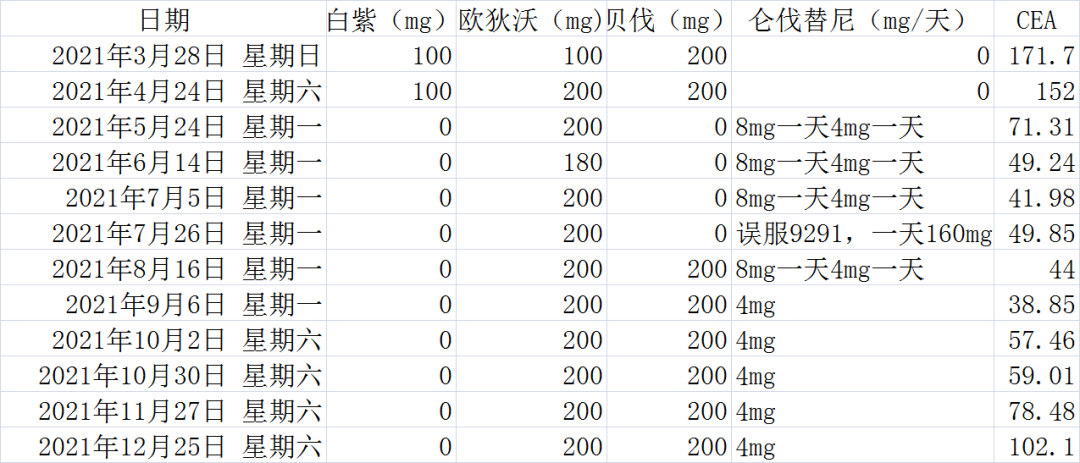
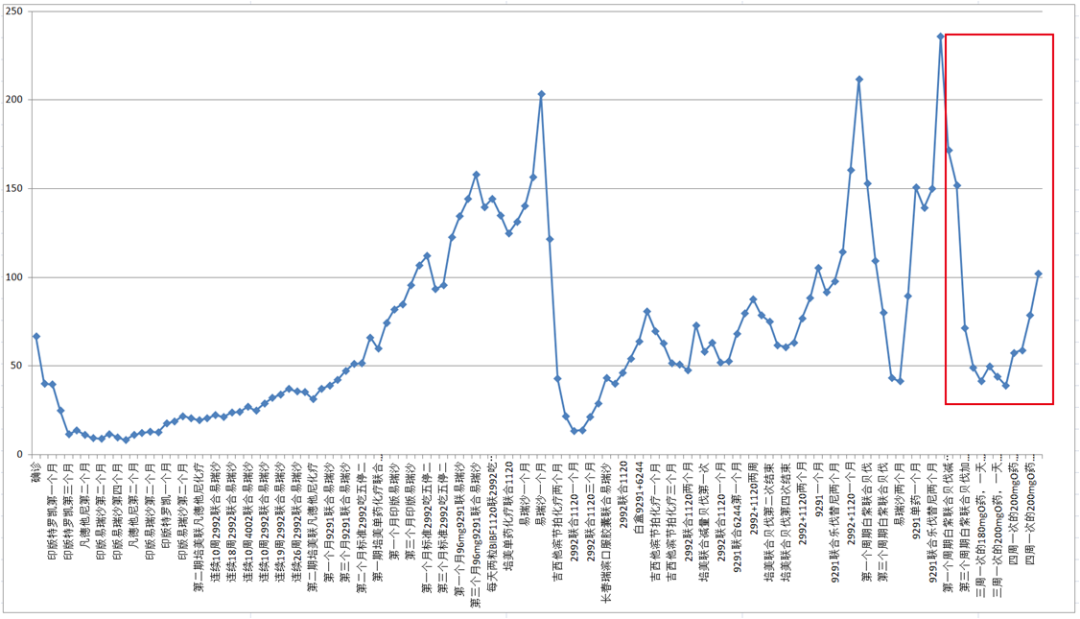
The red box in the CEA trend chart shows the changes in CEA during immunotherapy in 2021
Additionally, before and after the immunotherapy in 2021, peripheral blood was sent for ctDNA testing, both times only showing the 19 deletion mutation, with abundance increasing from 0.31% on March 3 to 0.38% on December 26, with no other mutations detected. (Click the image to enlarge)

Appendix 2: Summary of Keenman’s Mother’s Treatment (Click the image to enlarge)
Previous Highlights | Other Articles by Super Moderator Keenman
Keenman: My Mother’s Five-Year Rebirth (Part 1)
Keenman: My Mother’s Five-Year Rebirth (Part 2)
Crossing Five Years | Breaking Through Six Years of Survival, Becoming One of the Lucky Few (Part 1)
Crossing Five Years | Breaking Through Six Years of Survival, Becoming One of the Lucky Few (Part 2)
Crossing Seven Years | Moderator Keenman’s Experience on Long-Term Cancer Survival
Crossing Eight Years | The “Three-Five-Seven” Rule of Cancer Victors
Crossing Nine Years | Persistence Brings Hope
Crossing Ten Years | From a Desired Dream to a Miracle Realized
Listening to Thunder in Silence: Experiences and Lessons in Managing Acute Interstitial Pneumonia
Star mark to follow, don’t miss out on exciting content!


Dancing with Cancer
Scan to add Dancing with Cancer Assistant
Help you find the organization and join the group for communication

