Insomnia is a common clinical condition. Over the years, I have encountered numerous cases of insomnia. Some treatments have been effective, while others have not met expectations. Through continuous practical experience, I have found that the efficacy ultimately comes from accurate differential diagnosis and treatment. Especially in clinical practice, one must forget the term “insomnia” and the concept of “heart-kidney interaction.” It is essential to use the appropriate herbs for the specific syndrome to achieve therapeutic results.
Let us look at a case.

This patient was referred by a friend. They suffer from chronic insomnia and have consulted many renowned doctors. They feel quite troubled and even a bit hopeless. Upon pulse diagnosis, I found the cun (寸) pulse to be deep and strong, while the chi (尺) pulse was deep, thin, and slightly rough. As shown in the image below:
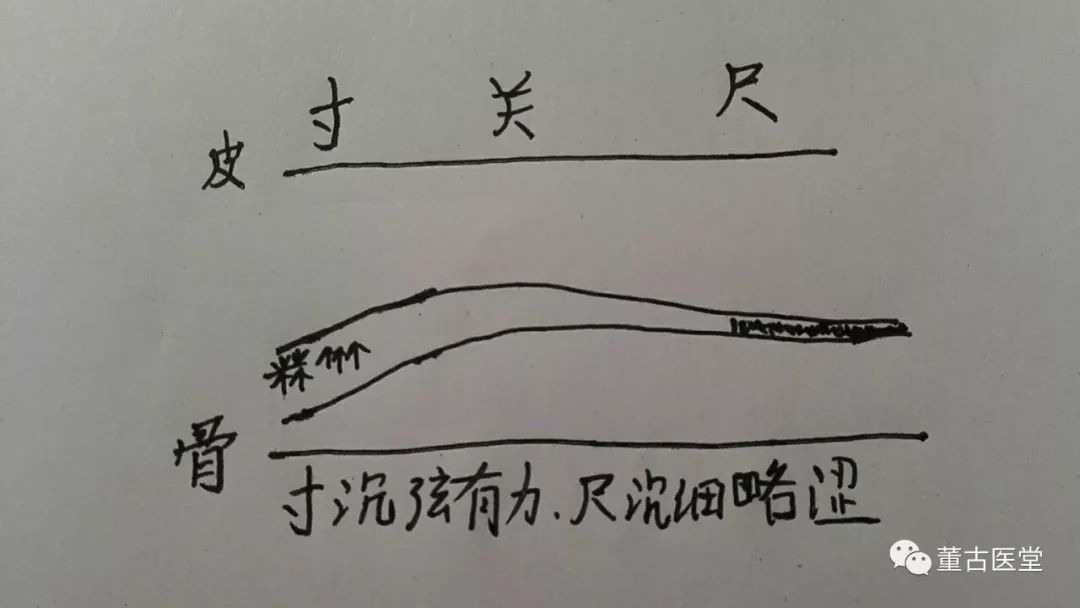
The strong deep cun pulse indicates the presence of internal water retention. The deep, thin, and rough chi pulse suggests a deficiency of blood and the presence of blood stasis. We can determine the nature of the pathogenic factors from the strong pulse and the condition of qi and blood from the weak pulse. Clearly, this is a condition characterized by heavy water retention and deficiency of blood with stasis. The strong cun pulse may be masking the thin and rough chi pulse.
Excessive water retention in the chest and insufficient blood nourishment can lead to anxiety, while blood stasis can cause vivid dreams; this is the pathogenesis.
Therefore, I prescribed Ling Gui Zhu Gan Tang (Poria, Cinnamon, Atractylodes, and Licorice Decoction) to address the water retention in the upper jiao and Xue Fu Zhu Yu Tang (Blood Mansion Decoction) to address the blood stasis and deficiency. The combination of these two formulas also has the effect of Dang Gui Shao Yao San (Angelica and Peony Powder).
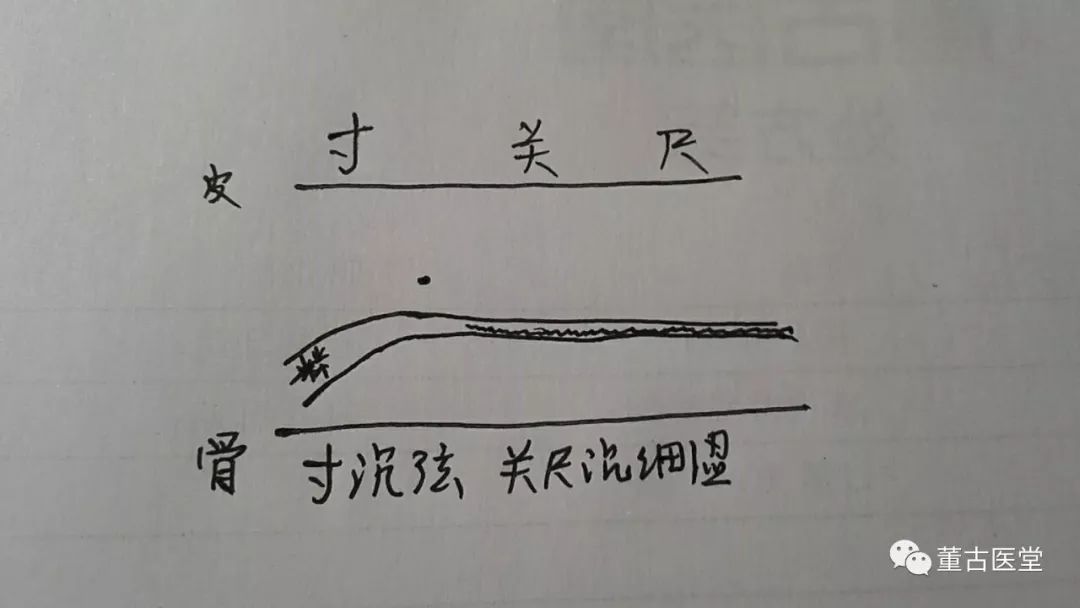
About a week later, the patient returned for a follow-up. Their sleep had improved, but they reported slight anxiety. The cun pulse remained deep and strong, the guan (关) pulse was slightly strong, and the chi pulse was deep, thin, and rough. As shown below:

The strong cun pulse and slight anxiety may indicate some mild internal heat. I added Ma Huang (Ephedra) and Shi Gao (Gypsum) to disperse this heat. Additionally, I included Xiang Fu (Cyperus) and Wu Yao (Lindera) to strengthen the regulation of qi, and Wu Ling Zhi (Flying Squirrel Feces) and Dan Pi (Moutan) to enhance the removal of stasis.
For patients with a strong cun pulse and anxiety, I personally prefer to add a small amount of Ma Huang and Shi Gao combined with Si Ni San (Frigid Extremities Powder) to disperse the internal heat.
A week later, the patient returned for another follow-up. Their sleep continued to improve. The cun pulse was still deep and strong, while the chi pulse was deep, thin, and rough. The chi pulse had transitioned from strong to deep and thin, likely due to the effects of Si Ni San combined with Ma Huang and Shi Gao in dispelling the stagnant qi and heat. The pulse image is shown below:
For treatment, I focused on the thin and rough chi pulse and prescribed Dang Gui Si Ni Tang (Angelica Frigid Extremities Decoction). As shown below:

After taking the medication this time, the patient reported that their sleep was completely restored. They later requested treatment for their scanty menstruation. As shown below:

After taking the medication for a while, the patient became a bit apprehensive about taking more medicine. They were very anxious and kept requesting to adjust their scanty menstruation quickly to see results. I was also pressured and felt troubled. In the next consultation, I directly used Gui Fu Di Huang Wan (Cinnamon and Atractylodes Pill) for their soft and weak lower abdomen. However, this led to gastrointestinal discomfort for the patient. Subsequently, the patient became fearful of taking medicine and did not continue with the treatment.
Now reflecting on this, I believe that in clinical practice, one should not rush with the patient’s anxiety. At that time, I should have continued with Ling Gui Zhu Gan Tang, Xue Fu Zhu Yu Tang, and Dang Gui Si Ni Tang as the main treatment, gradually adding qi and blood tonics. Perhaps this more cautious and gradual approach would have achieved results more quickly.
Welcome to exchange and correct me, fellow practitioners!
Dr. Dong (WeChat ID: 13310830760)