Introduction: Many stroke patients clinically experience sleep disorders and frequent nocturia, presenting with a pulse of excess above and deficiency below. By employing the method of nourishing the heart and consolidating the kidneys, patients’ sleep can improve, and nocturia can decrease.

Case One
A 74-year-old female, medical record number 2024100364.
Admitted for “dizziness accompanied by nausea and vomiting, and limb weakness for 1 month,” diagnosed with hemiplegia, cerebral infarction; posterior circulation ischemia, hypertension; dysphagia; type 2 diabetes; atrial fibrillation; sleep disorders. Blood sugar controlled long-term with insulin and oral medications. Very little staple food intake.
On November 18, 2024, the patient developed low fever, throat discomfort, and a cough with little phlegm. Due to elevated white blood cells and neutrophil C-reactive protein, she was treated with fluid replacement and anti-infection therapy. After stopping fluid replacement and anti-infection treatment on the 29th, she still had clear nasal discharge, cough with little phlegm, difficulty swallowing, no headache, dizziness when turning her head in bed but not when still, no nausea or vomiting, good appetite, no feeling of fullness, hard stools, and had not defecated for 5 days, reporting that she had loose stools 2 days after anti-infection treatment.
Afraid of wind and cold, no sweating, no limb pain or numbness, hands and feet warm.History of dysphagia.
The tongue was slightly red, with a white coating that was not thick or greasy,the left pulse was slippery and slightly rough at the cun position, deep and wiry at the guan position, and deep at the chi position; the right pulse was deep and did not respond to the fingers.
History of intermittent atrial fibrillation, currently taking amiodarone.
Considering a combined exterior-interior disease, with exterior wind-cold-damp unresolved, and lung function impaired, treated with a modified Zhi Sou San (Stop Cough Powder) combined with Shen Su Yin (Ginseng and Astragalus Decoction).
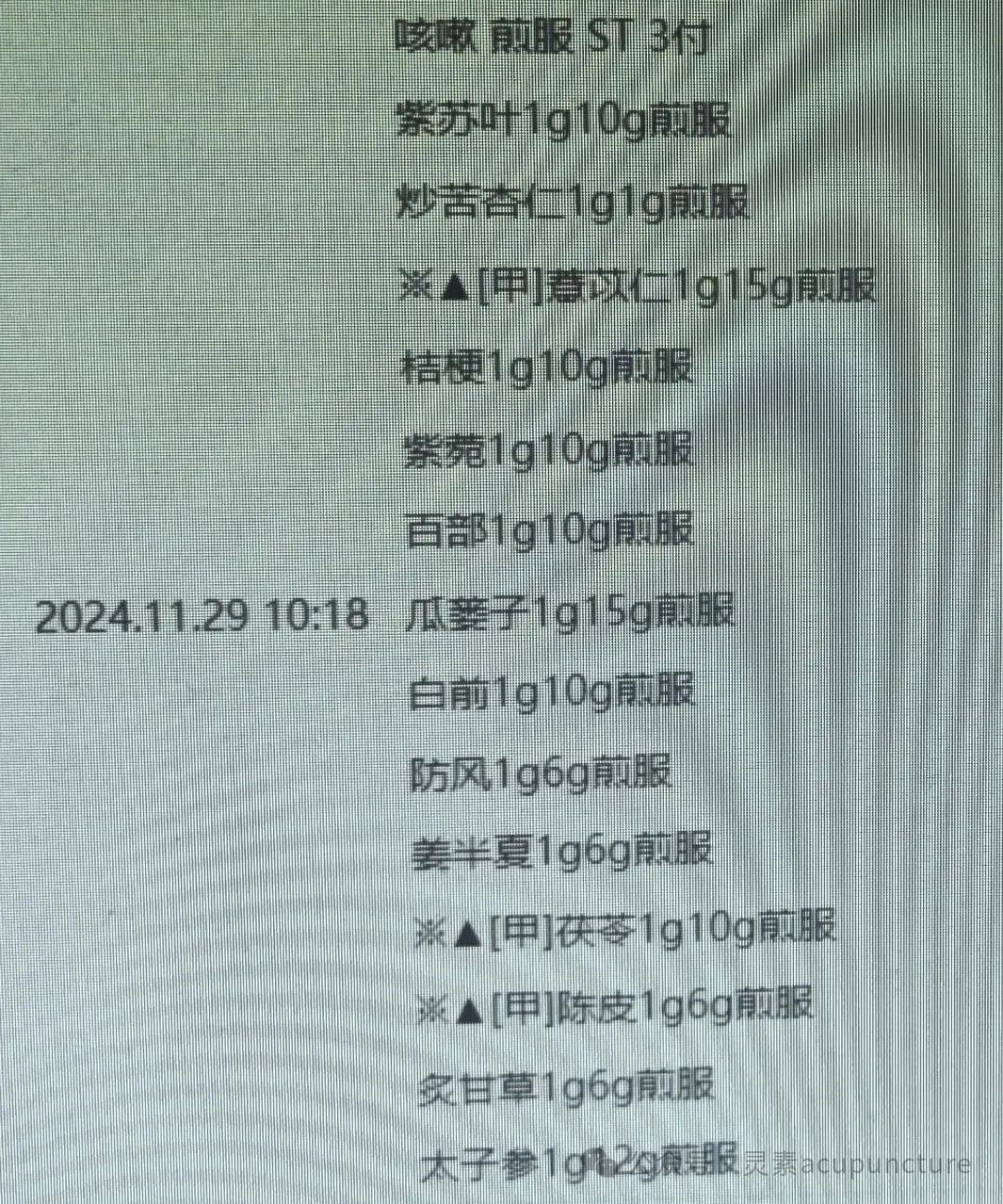
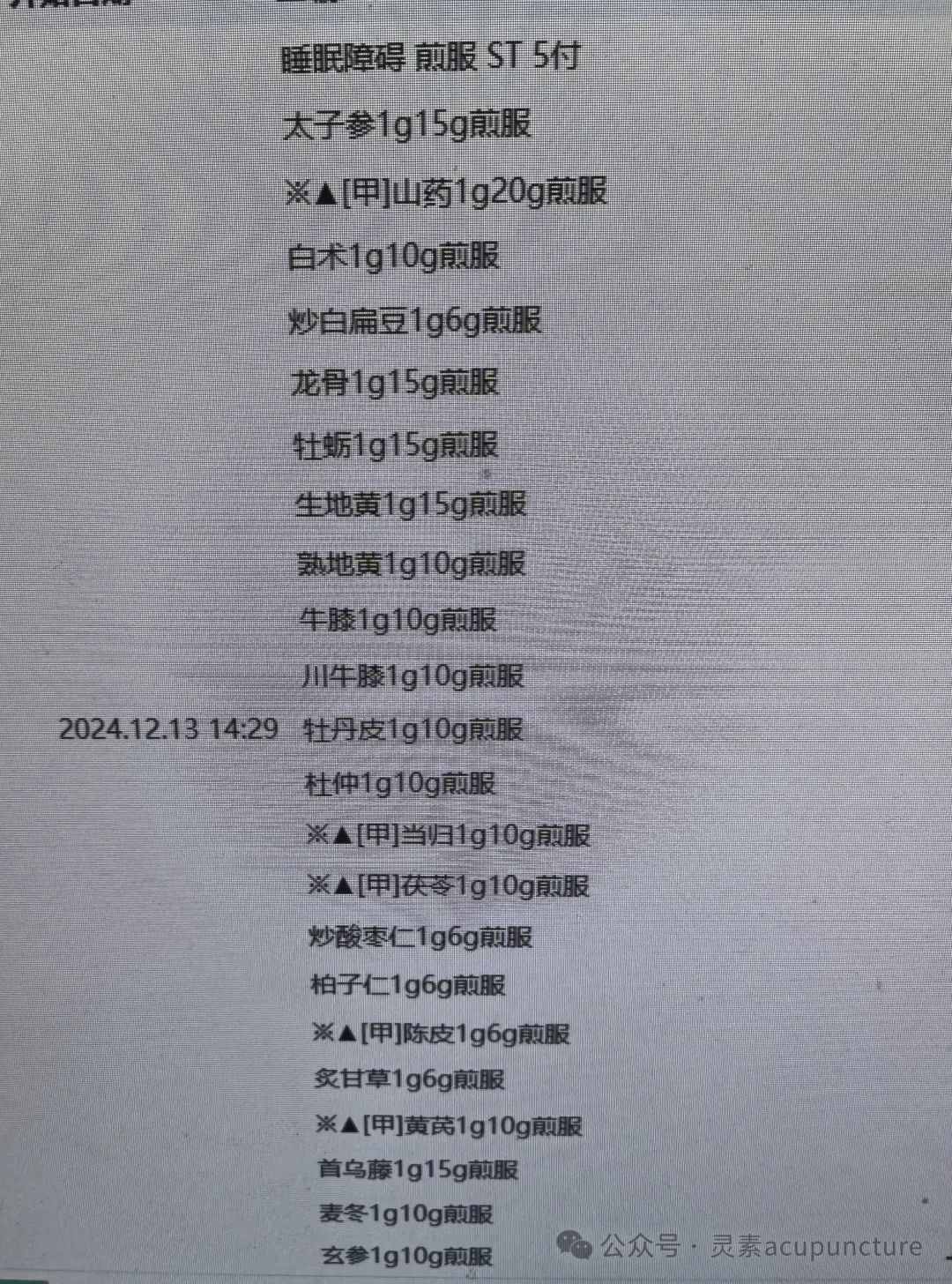
On December 6, during rounds, the patient had a slight cough with little phlegm, no chest tightness or shortness of breath, no palpitations, good appetite, but ate little due to fear of blood sugar rising, blood sugar unstable, fluctuating high and low, sleep at night was average, did not want to drink water, urination during the day was acceptable, frequent nocturia, hard stools. The tongue was slightly red with little coating,the left pulse was floating and slippery at the cun position, deep at the guan and chi positions, the right pulse was deep and did not respond to the fingers. Considering spleen and stomach qi and yin deficiency, and heart and liver deficiency, treated with a decoction of Chinese herbs to tonify qi and yin, nourish the heart and kidneys, and stabilize and descend, supplemented with lung qi dispersing. The formula included: Tai Zi Shen (Pseudostellaria) 15g, Shan Yao (Chinese Yam) 20g, Bai Zhu (White Atractylodes) 10g, Chao Bai Bian Dou (Fried Hyacinth Bean) 6g, Long Gu (Dragon Bone) 15g, Mu Li (Oyster Shell) 15g, Sheng Di Huang (Raw Rehmannia) 10g, Shu Di Huang (Prepared Rehmannia) 10g, Chuan Niu Xi (Chinese Achyranthes) 10g, Mu Dan Pi (Moutan Root) 10g, Du Zhong (Eucommia) 10g, Dang Gui (Angelica) 10g, Fu Ling (Poria) 10g, Chao Suan Zao Ren (Fried Sour Jujube Seed) 6g, Bai Zi Ren (Arborvitae Seed) 6g, Chen Pi (Tangerine Peel) 6g, Zhi Gan Cao (Honey-Fried Licorice) 6g, Jie Geng (Platycodon) 6g, Zi Wan (Aster) 10g, Bai Bu (Stemona) 10g, 5 doses, decocted and taken warm, 1 dose per day. On December 13, during rounds, there were no respiratory symptoms, nocturia reduced to 4-5 times, sleep was average.
 On December 20, during rounds, the patient’s blood sugar was stable recently, sleep at night was good, and nocturia significantly reduced, the tongue was slightly red, with less coating, the pulsewas floating and reduced at the left cun position, slightly slippery, deep at the guan and chi positions, the right pulse was deep, continued with oral Chinese medicine to tonify qi, strengthen the spleen, and nourish the heart, and to tonify the liver and kidneys. The formula included: Tai Zi Shen (Pseudostellaria) 15g, Shan Yao (Chinese Yam) 20g, Bai Zhu (White Atractylodes) 10g, Chao Bai Bian Dou (Fried Hyacinth Bean) 10g, Long Gu (Dragon Bone) 15g, Mu Li (Oyster Shell) 15g, Sheng Di Huang (Raw Rehmannia) 15g, Shu Di Huang (Prepared Rehmannia) 10g, Niu Xi (Achyranthes) 10g, Chuan Niu Xi (Chinese Achyranthes) 10g, Dan Pi (Moutan Root) 10g, Du Zhong (Eucommia) 10g, Dang Gui (Angelica) 10g, Fu Ling (Poria) 10g, Chao Suan Zao Ren (Fried Sour Jujube Seed) 6g, Bai Zi Ren (Arborvitae Seed) 6g, Chen Pi (Tangerine Peel) 6g, Zhi Gan Cao (Honey-Fried Licorice) 6g, Huang Qi (Astragalus) 10g, He Shou Wu (Fo-Ti) 15g, Mai Dong (Ophiopogon) 10g, Xuan Shen (Scrophularia) 10g, 7 doses, decocted and taken warm, 1 dose per day. On December 27, during rounds, sleep at night was good, nocturia reduced to 2-3 times. Blood sugar control was stable. The left cun pulse was slippery but not floating, deep at the guan and chi positions, the right pulse was deep.
On December 20, during rounds, the patient’s blood sugar was stable recently, sleep at night was good, and nocturia significantly reduced, the tongue was slightly red, with less coating, the pulsewas floating and reduced at the left cun position, slightly slippery, deep at the guan and chi positions, the right pulse was deep, continued with oral Chinese medicine to tonify qi, strengthen the spleen, and nourish the heart, and to tonify the liver and kidneys. The formula included: Tai Zi Shen (Pseudostellaria) 15g, Shan Yao (Chinese Yam) 20g, Bai Zhu (White Atractylodes) 10g, Chao Bai Bian Dou (Fried Hyacinth Bean) 10g, Long Gu (Dragon Bone) 15g, Mu Li (Oyster Shell) 15g, Sheng Di Huang (Raw Rehmannia) 15g, Shu Di Huang (Prepared Rehmannia) 10g, Niu Xi (Achyranthes) 10g, Chuan Niu Xi (Chinese Achyranthes) 10g, Dan Pi (Moutan Root) 10g, Du Zhong (Eucommia) 10g, Dang Gui (Angelica) 10g, Fu Ling (Poria) 10g, Chao Suan Zao Ren (Fried Sour Jujube Seed) 6g, Bai Zi Ren (Arborvitae Seed) 6g, Chen Pi (Tangerine Peel) 6g, Zhi Gan Cao (Honey-Fried Licorice) 6g, Huang Qi (Astragalus) 10g, He Shou Wu (Fo-Ti) 15g, Mai Dong (Ophiopogon) 10g, Xuan Shen (Scrophularia) 10g, 7 doses, decocted and taken warm, 1 dose per day. On December 27, during rounds, sleep at night was good, nocturia reduced to 2-3 times. Blood sugar control was stable. The left cun pulse was slippery but not floating, deep at the guan and chi positions, the right pulse was deep. On December 29, stable discharge.
On December 29, stable discharge. Case Two A 66-year-old male, medical record number 2024100381, admitted for “difficulty in movement of the right limbs accompanied by unclear speech for 8 months.” Diagnosed with hemiplegia, sequelae of cerebral infarction; speech disorder; hypertension; type 2 diabetes; peripheral neuropathy due to type 2 diabetes; epilepsy; post-stenting of left middle cerebral artery stenosis; right internal carotid artery stenosis. Long-term subcutaneous injection of insulin glargine, currently at 8 units. Hydrochloride of etizolam has been used since September. On December 9, during rounds, the patient’s general condition was acceptable, the right limbs had difficulty moving, upper limb muscle tone was slightly high, lower limb was acceptable, speech was slurred, left hand easily sweated, recent fasting blood sugar was slightly low, felt dry mouth, diet was acceptable, bowel movements were self-initiated, urination was excessive, sleep was restless, the tongue tip was red, with a slightly thick white coating in the middle and back,the left pulse was floating and slippery at the cun position, deep at the guan and chi positions, the right pulse was wiry and rough. Based on the above symptoms and signs, diagnosed with stroke syndrome of yin deficiency and damp-heat, treated with a modified Jian Ling Tang (Building Spirit Decoction) combined with Di Huang Yin Zi (Rehmannia Decoction). The remaining treatment was the same as before. Acupuncture was performed twice a week. The herbal prescription included: Long Gu (Dragon Bone) 15g, Mu Li (Oyster Shell) 15g, Sheng Di Huang (Raw Rehmannia) 10g, Yi Ren (Job’s Tears) 10g, Shan Yao (Chinese Yam) 10g, Dan Pi (Moutan Root) 10g, Fu Ling (Poria) 15g, Ze Xie (Alisma) 10g, Mai Dong (Ophiopogon) 10g, Wu Wei Zi (Schisandra) 3g, Shi Chang Pu (Acorus) 10g, Yuan Zhi (Polygala) 6g, Rou Cong Rong (Cistanche) 10g, Ba Ji Tian (Morinda) 10g, Bo He (Mint) 6g, He Shou Wu (Fo-Ti) 15g, Ji Xue Teng (Spatholobus) 15g, Bai Zi Ren (Arborvitae Seed) 10g, Du Zhong (Eucommia) 10g, Niu Xi (Achyranthes) 10g, Chuan Niu Xi (Chinese Achyranthes) 10g, Cang Zhu (Atractylodes) 6g, Bai Zhu (White Atractylodes) 10g, Dang Shen (Codonopsis) 10g, Fa Ban Xia (Pinellia) 6g, Chen Pi (Tangerine Peel) 6g, 7 doses, decocted and taken warm, 1 dose per day. On December 16, during rounds, the patient’s right limb muscle tone decreased, speech remained slurred, left hand showed no significant sweating, fasting blood sugar was low, felt dry mouth, diet was acceptable, bowel movements were self-initiated, urination was excessive, sleep improved compared to before, the tongue tip was red, with a slightly thick white coating,the left pulse was slightly floating and slippery, deep at the guan and chi positions, the right pulse was wiry and fine. The next day, after adjusting the herbal medicine, the patient’s fasting blood sugar decreased, considering it was due to the oral Chinese medicine, continued to observe, and reduce insulin dosage if necessary.
Case Two A 66-year-old male, medical record number 2024100381, admitted for “difficulty in movement of the right limbs accompanied by unclear speech for 8 months.” Diagnosed with hemiplegia, sequelae of cerebral infarction; speech disorder; hypertension; type 2 diabetes; peripheral neuropathy due to type 2 diabetes; epilepsy; post-stenting of left middle cerebral artery stenosis; right internal carotid artery stenosis. Long-term subcutaneous injection of insulin glargine, currently at 8 units. Hydrochloride of etizolam has been used since September. On December 9, during rounds, the patient’s general condition was acceptable, the right limbs had difficulty moving, upper limb muscle tone was slightly high, lower limb was acceptable, speech was slurred, left hand easily sweated, recent fasting blood sugar was slightly low, felt dry mouth, diet was acceptable, bowel movements were self-initiated, urination was excessive, sleep was restless, the tongue tip was red, with a slightly thick white coating in the middle and back,the left pulse was floating and slippery at the cun position, deep at the guan and chi positions, the right pulse was wiry and rough. Based on the above symptoms and signs, diagnosed with stroke syndrome of yin deficiency and damp-heat, treated with a modified Jian Ling Tang (Building Spirit Decoction) combined with Di Huang Yin Zi (Rehmannia Decoction). The remaining treatment was the same as before. Acupuncture was performed twice a week. The herbal prescription included: Long Gu (Dragon Bone) 15g, Mu Li (Oyster Shell) 15g, Sheng Di Huang (Raw Rehmannia) 10g, Yi Ren (Job’s Tears) 10g, Shan Yao (Chinese Yam) 10g, Dan Pi (Moutan Root) 10g, Fu Ling (Poria) 15g, Ze Xie (Alisma) 10g, Mai Dong (Ophiopogon) 10g, Wu Wei Zi (Schisandra) 3g, Shi Chang Pu (Acorus) 10g, Yuan Zhi (Polygala) 6g, Rou Cong Rong (Cistanche) 10g, Ba Ji Tian (Morinda) 10g, Bo He (Mint) 6g, He Shou Wu (Fo-Ti) 15g, Ji Xue Teng (Spatholobus) 15g, Bai Zi Ren (Arborvitae Seed) 10g, Du Zhong (Eucommia) 10g, Niu Xi (Achyranthes) 10g, Chuan Niu Xi (Chinese Achyranthes) 10g, Cang Zhu (Atractylodes) 6g, Bai Zhu (White Atractylodes) 10g, Dang Shen (Codonopsis) 10g, Fa Ban Xia (Pinellia) 6g, Chen Pi (Tangerine Peel) 6g, 7 doses, decocted and taken warm, 1 dose per day. On December 16, during rounds, the patient’s right limb muscle tone decreased, speech remained slurred, left hand showed no significant sweating, fasting blood sugar was low, felt dry mouth, diet was acceptable, bowel movements were self-initiated, urination was excessive, sleep improved compared to before, the tongue tip was red, with a slightly thick white coating,the left pulse was slightly floating and slippery, deep at the guan and chi positions, the right pulse was wiry and fine. The next day, after adjusting the herbal medicine, the patient’s fasting blood sugar decreased, considering it was due to the oral Chinese medicine, continued to observe, and reduce insulin dosage if necessary. 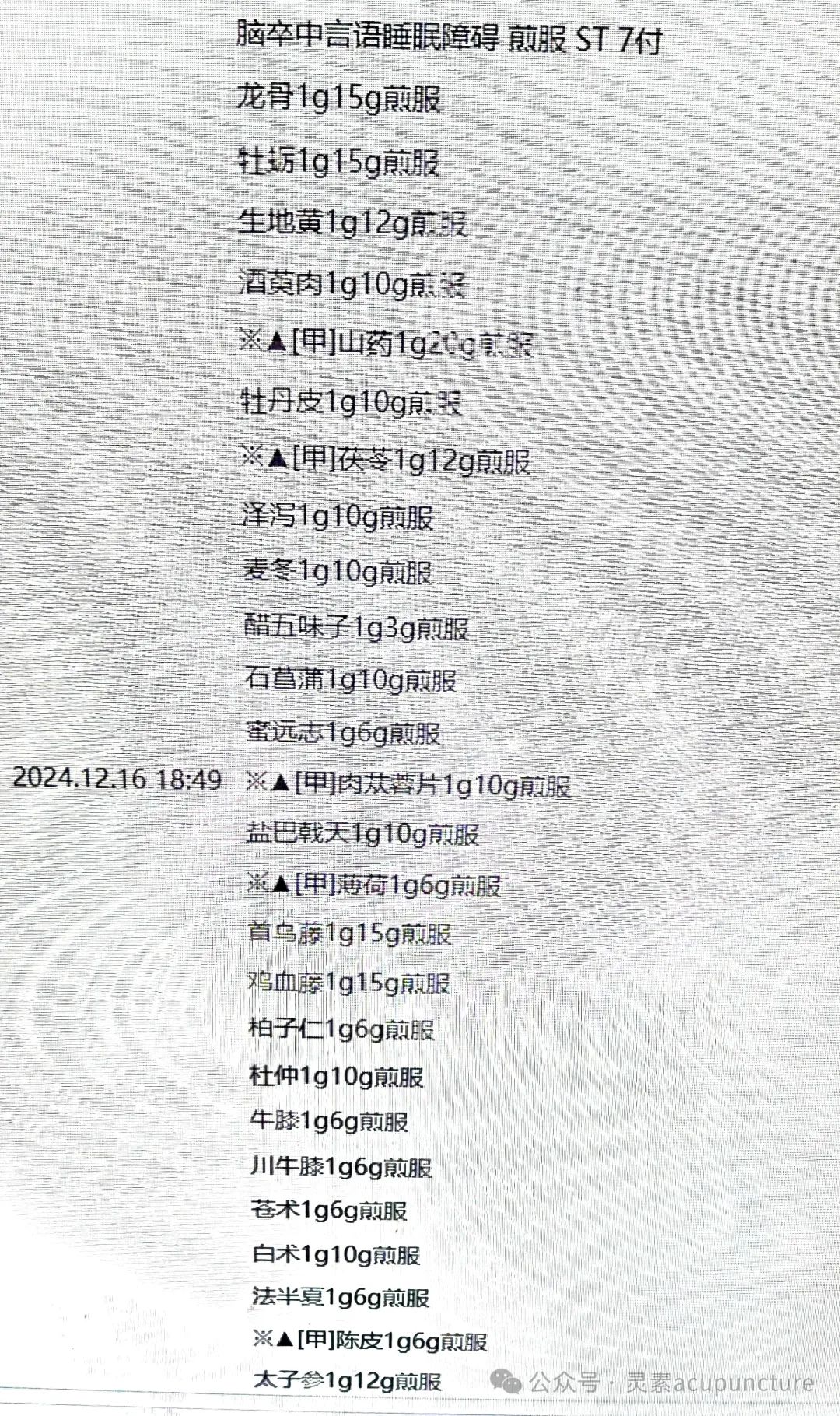 On December 23, sleep continued to improve, urination was excessive improved to about 2 times at night. Left limb muscle tone was basically normal, blood sugar was stable, insulin reduced to 6 units. The formula included: Mu Li (Oyster Shell) 15g, Sheng Di Huang (Raw Rehmannia) 12g, Yi Ren (Job’s Tears) 10g, Shan Yao (Chinese Yam) 20g, Dan Pi (Moutan Root) 10g, Fu Ling (Poria) 12g, Ze Xie (Alisma) 10g, Mai Dong (Ophiopogon) 10g, Wu Wei Zi (Schisandra) 6g, Shi Chang Pu (Acorus) 10g, Yuan Zhi (Polygala) 6g, Bo He (Mint) 6g, He Shou Wu (Fo-Ti) 15g, Ji Xue Teng (Spatholobus) 15g, Du Zhong (Eucommia) 10g, Niu Xi (Achyranthes) 6g, Chuan Niu Xi (Chinese Achyranthes) 6g, Cang Zhu (Atractylodes) 6g, Bai Zhu (White Atractylodes) 10g, Fa Ban Xia (Pinellia) 6g, Chen Pi (Tangerine Peel) 6g, Tai Zi Shen (Pseudostellaria) 12g, Dan Shen (Salvia) 10g, Ba Ji Tian (Morinda) 10g, Rou Cong Rong (Cistanche) 10g, Zhen Zhu Mu (Mother of Pearl) 20g, Bai Zi Ren (Arborvitae Seed) 6g, 7 doses, decocted and taken warm, 1 dose per day. On January 6, during rounds, all symptoms were stable, daytime urination was slightly more, the tongue edges were still red, with a slightly thick white coating in the middle and back, the left pulse was slightly slippery, soft and wiry at the guan position, the right pulse was slightly wiry and rough. Continued with oral Chinese medicine. Yi Ren (Job’s Tears) 10g, Fu Ling (Poria) 12g, Mai Dong (Ophiopogon) 10g, vinegar Wu Wei Zi (Schisandra) 3g, Shi Chang Pu (Acorus) 10g, Yuan Zhi (Polygala) 6g, He Shou Wu (Fo-Ti) 10g, Ji Xue Teng (Spatholobus) 10g, Du Zhong (Eucommia) 10g, Niu Xi (Achyranthes) 6g, Chuan Niu Xi (Chinese Achyranthes) 6g, Cang Zhu (Atractylodes) 6g, Bai Zhu (White Atractylodes) 10g, Chen Pi (Tangerine Peel) 6g, Dan Shen (Salvia) 10g, Ba Ji Tian (Morinda) 10g, Rou Cong Rong (Cistanche) 10g, Shan Yao (Chinese Yam) 15g, Huang Qi (Astragalus) 10g, Zhen Zhu Mu (Mother of Pearl) 20g, Zhi Gan Cao (Honey-Fried Licorice) 6g, Dang Gui (Angelica) 10g, Shu Di Huang (Prepared Rehmannia) 10g, Sheng Di Huang (Raw Rehmannia) 10g, Dang Shen (Codonopsis) 6g, Long Yan Rou (Longan) 10g, Yan Yi Zhi Ren (Alpinia) 6g, Gou Qi Zi (Goji Berries) 10g, 7 doses, decocted and taken warm, 1 dose per day. On January 7, the endocrinology department consulted, insulin was stopped, and oral medications were used to control blood sugar. On January 13, during rounds, sleep was normal, nocturia was 1-2 times, daytime urination frequency decreased, blood sugar was stable, the tongue edges were still red, with a slightly thick white coating, the left pulse was deep, soft and wiry at the guan position, the right pulse was slightly wiry and slippery. Continued with oral Chinese medicine. Subsequently, nighttime sleep was basically normal, nocturia was about once, daytime urination was about 3-5 times. The left cun pulse was soft and slippery, the guan position was still wiry, but stronger than before, and the patient was discharged with stable medication before the New Year.
On December 23, sleep continued to improve, urination was excessive improved to about 2 times at night. Left limb muscle tone was basically normal, blood sugar was stable, insulin reduced to 6 units. The formula included: Mu Li (Oyster Shell) 15g, Sheng Di Huang (Raw Rehmannia) 12g, Yi Ren (Job’s Tears) 10g, Shan Yao (Chinese Yam) 20g, Dan Pi (Moutan Root) 10g, Fu Ling (Poria) 12g, Ze Xie (Alisma) 10g, Mai Dong (Ophiopogon) 10g, Wu Wei Zi (Schisandra) 6g, Shi Chang Pu (Acorus) 10g, Yuan Zhi (Polygala) 6g, Bo He (Mint) 6g, He Shou Wu (Fo-Ti) 15g, Ji Xue Teng (Spatholobus) 15g, Du Zhong (Eucommia) 10g, Niu Xi (Achyranthes) 6g, Chuan Niu Xi (Chinese Achyranthes) 6g, Cang Zhu (Atractylodes) 6g, Bai Zhu (White Atractylodes) 10g, Fa Ban Xia (Pinellia) 6g, Chen Pi (Tangerine Peel) 6g, Tai Zi Shen (Pseudostellaria) 12g, Dan Shen (Salvia) 10g, Ba Ji Tian (Morinda) 10g, Rou Cong Rong (Cistanche) 10g, Zhen Zhu Mu (Mother of Pearl) 20g, Bai Zi Ren (Arborvitae Seed) 6g, 7 doses, decocted and taken warm, 1 dose per day. On January 6, during rounds, all symptoms were stable, daytime urination was slightly more, the tongue edges were still red, with a slightly thick white coating in the middle and back, the left pulse was slightly slippery, soft and wiry at the guan position, the right pulse was slightly wiry and rough. Continued with oral Chinese medicine. Yi Ren (Job’s Tears) 10g, Fu Ling (Poria) 12g, Mai Dong (Ophiopogon) 10g, vinegar Wu Wei Zi (Schisandra) 3g, Shi Chang Pu (Acorus) 10g, Yuan Zhi (Polygala) 6g, He Shou Wu (Fo-Ti) 10g, Ji Xue Teng (Spatholobus) 10g, Du Zhong (Eucommia) 10g, Niu Xi (Achyranthes) 6g, Chuan Niu Xi (Chinese Achyranthes) 6g, Cang Zhu (Atractylodes) 6g, Bai Zhu (White Atractylodes) 10g, Chen Pi (Tangerine Peel) 6g, Dan Shen (Salvia) 10g, Ba Ji Tian (Morinda) 10g, Rou Cong Rong (Cistanche) 10g, Shan Yao (Chinese Yam) 15g, Huang Qi (Astragalus) 10g, Zhen Zhu Mu (Mother of Pearl) 20g, Zhi Gan Cao (Honey-Fried Licorice) 6g, Dang Gui (Angelica) 10g, Shu Di Huang (Prepared Rehmannia) 10g, Sheng Di Huang (Raw Rehmannia) 10g, Dang Shen (Codonopsis) 6g, Long Yan Rou (Longan) 10g, Yan Yi Zhi Ren (Alpinia) 6g, Gou Qi Zi (Goji Berries) 10g, 7 doses, decocted and taken warm, 1 dose per day. On January 7, the endocrinology department consulted, insulin was stopped, and oral medications were used to control blood sugar. On January 13, during rounds, sleep was normal, nocturia was 1-2 times, daytime urination frequency decreased, blood sugar was stable, the tongue edges were still red, with a slightly thick white coating, the left pulse was deep, soft and wiry at the guan position, the right pulse was slightly wiry and slippery. Continued with oral Chinese medicine. Subsequently, nighttime sleep was basically normal, nocturia was about once, daytime urination was about 3-5 times. The left cun pulse was soft and slippery, the guan position was still wiry, but stronger than before, and the patient was discharged with stable medication before the New Year.
 ▶ Disclaimer:
▶ Disclaimer:
The articles written are for learning and communication purposes only. Non-professionals in Traditional Chinese Medicine should not blindly try medications; please conduct reasonable treatment under the guidance of professionals. The views in the article are for clinical thought reference only.

