Guidewire serves the purpose of providing a “track” for subsequent instruments such as balloons, stents, ultrasound catheters, and rotational heads to enter the diseased blood vessels through the site of coronary artery stenosis or occlusion. Therefore, the guidewire is an essential instrument in coronary interventional therapy.
Correctly selecting and operating the guidewire through the lesion site is a necessary condition for the success of interventional therapy, especially when treating chronic occlusive lesions, bifurcation lesions, and extremely tortuous or angulated lesions. The choice and operational skills of the guidewire largely determine whether the interventional procedure can be successful. Thus, understanding the characteristics and classifications of guidewires and correctly selecting and operating them during surgery is a fundamental skill that coronary interventionalists need to master.
1
Structural Characteristics of Guidewires
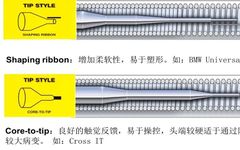
The guidewires currently in use have a body diameter of 0.014 inches, typically composed of proximal push rod, core wire, core wire transition section, and guidewire tip. The outer surface of the guidewire tip has a sheath and coating (Figure 1).
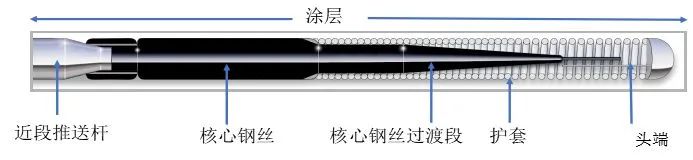
Figure 1 Guidewire Structure Diagram
The core wire runs through the entire length of the guidewire, appearing as a uniform cylinder in the proximal push rod section, and gradually tapering in the transition section near the tip. This part is the core of the guidewire design, and the length and transition method of the transition section determine the guidewire’s support, torque control, pushability, and flexibility. The thicker the core wire, the greater the hardness of the guidewire and the lesser its flexibility. A longer transition section design provides better flexibility, making it easier to navigate through tortuous vessels and collateral vessels. The design and structure of the tip is the most complex part of the guidewire design, generally having two structural designs: the first is a core wire that gradually tapers to the tip (Core-to-Tip); the second design has the core wire not reaching the tip, with a separately manufactured tip welded to the end of the core wire (Shaping Ribbon, Figure 2).
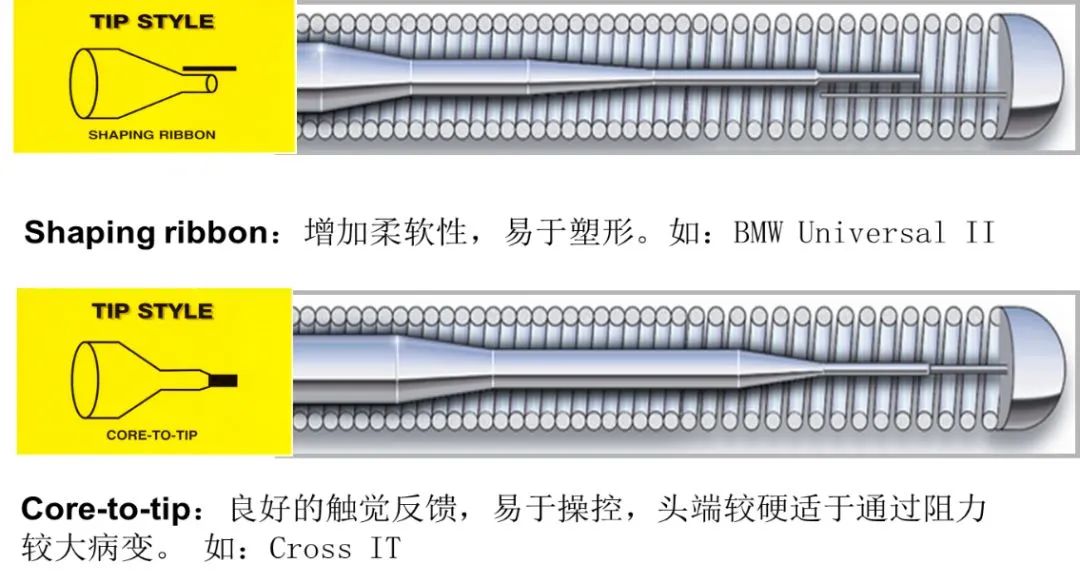
Figure 2 Guidewire Tip Design
Regardless of the design, the guidewire tip’s wire is very thin and needs to be covered with a sheath to prevent damage, and the sheath allows the tip’s diameter to match the body at 0.014 inches (conical guidewires can be less than 0.014 inches). The tip sheath comes in two materials: polymer sheath and spring coil (or wrapped wire) sheath (Figure 3). The polymer sheath has excellent hydrophilicity, reducing resistance when the guidewire passes through lesions; while the spring coil sheath provides better tactile feedback (i.e., the operator can feel the resistance encountered by the guidewire tip).
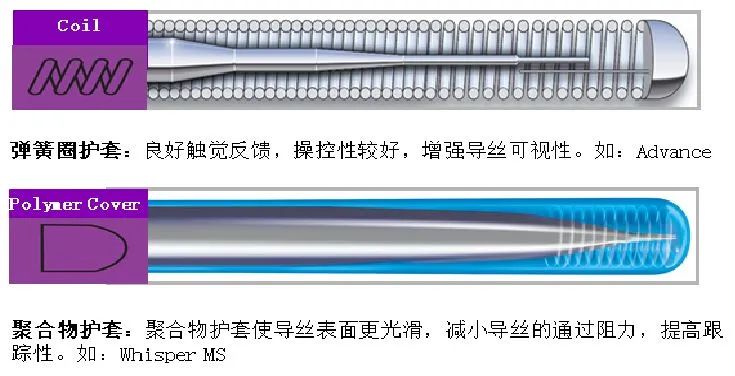
Figure 3 Guidewire Tip Sheath
The surface of the guidewire also has a thin coating to reduce friction and improve the interaction between instruments (balloon/guidewire, stent/guidewire), enhancing the guidewire’s tracking ability in the vessels, including hydrophilic and hydrophobic coatings. Hydrophilic coated guidewires attract water molecules to form a “gel-like” surface, reducing passage resistance. Hydrophobic coated guidewires resist water molecules to form a “waxy” surface, reducing friction and increasing the guidewire’s tracking ability.
2
Characteristics of Guidewires
The tip hardness, torque control, flexibility, support, pushability, visibility, and tactile feedback are several basic aspects reflecting the characteristics of guidewires. As an operator, a fundamental knowledge to understand is that there is no perfect guidewire suitable for all lesions; in practice, different guidewires with varying characteristics need to be selected based on different needs to complete interventional procedures.
Tip Hardness
Tip hardness refers to the ability of the guidewire tip to resist pressure while maintaining its normal shape. The greater the tip hardness, the stronger the guidewire’s ability to penetrate occlusive lesions, but this also increases the risk of vascular perforation. Traditionally, the hardness of the guidewire tip is divided into four levels, from the softest to the hardest: Floppy (Supersoft), Intermediate (Soft), Standard, and Standard Plus. In the past decade, with the continuous development of guidewires specifically for chronic total occlusion (CTO), the hardness of guidewire tips has become more diverse, and the traditional grading method cannot accurately define tip hardness. Currently, it is preferred to use “grams (g)” to indicate guidewire tip hardness, with the softest guidewire having a hardness of about 0.4g, while the hardest guidewire has a hardness of 20g. Most lesions can be addressed with guidewires having a tip hardness of less than 1g, while harder guidewires are mainly used for CTO lesions.
Torque Control
Torque control refers to the ability of the guidewire tip to follow the rotation of the proximal section (the external metal push rod section) when the operator rotates the proximal section, reflecting the flexibility of the guidewire tip under manual manipulation. The stronger the torque control, the better the guidewire’s ability to reach and cross lesions. The strength of torque control depends on the diameter of the core wire and the structure of the guidewire tip.
Flexibility
Flexibility refers to the guidewire’s ability to conform to the natural state of the vessel while passing through lesions. This is mainly determined by the diameter of the core wire, the structural form of the transition section, and the connection method between the core wire and the guidewire tip.
Support
Support refers to the ability of the guidewire to maintain stability in the vessel while serving as a delivery track for balloons or stents during the entry and passage of instruments through lesions. Generally speaking, support and flexibility are two opposing characteristics; guidewires with strong support tend to have poor flexibility, and vice versa.
Pushability
Pushability refers to the ability of the guidewire to pass through lesions under the influence of the operator’s external push rod. This depends on the hardness (diameter) of the core wire and the design of the transition section. If the core wire transition section is designed to taper gradually, the transmission of push force is more uniform, making it easier to navigate through tortuous and angulated vascular lesions compared to a stepped transition section design; soft guidewires with poor pushability are less likely to cause vascular perforation, making them safer to operate, while guidewires with strong pushability and harder tips are more likely to cause vascular dissection or perforation.
Visibility
Visibility refers to the length of the guidewire’s distal end that is radiolucent, helping the operator identify the guidewire’s direction and its position within the coronary lumen. Most guidewires have a visible segment length of 3 centimeters, but CTO-specific guidewires can have a visible segment length of up to 18 centimeters.
3
Classification of Guidewires
Guidewires can be classified in various ways, including classification by tip hardness, sheath type, and surface coating type, etc. Currently, the commonly used classification method divides guidewires into general-purpose guidewires and chronic total occlusion (CTO) guidewires.
General-purpose guidewires, also known as working guidewires, are primarily characterized by softer tip hardness, good torque control, and support, making them suitable for the vast majority of ordinary lesions and acute occlusive lesions. Representative guidewires include Abbott’s BMW series, Terumo’s Runthrough guidewires, Asahi’s Sion series, and Fielder FC guidewires.
Chronic total occlusion (CTO) guidewires are used to navigate through chronic occlusive lesions. Depending on the characteristics of the lesions, such as whether there is a tapered remnant at the proximal occlusion, the hardness of the fibrous cap, the length of the occlusion segment, and whether the occlusion segment is tortuous, many companies have designed CTO guidewires with different characteristics, which can be broadly categorized into several types:
(1) Ultra-slick guidewires, with Abbott’s Pilot series being the most representative, are mainly used to navigate through longer, tortuous CTO lesions;
(2) Puncture-type guidewires, which have a high tip hardness and can penetrate hard fibrous caps, such as Abbott’s Cross IT series, Asahi’s Miracle series, and Conquest series guidewires, are mainly used for CTO lesions with a proximal occlusion that lacks a tapered remnant, has a hard fibrous cap, but a shorter occlusion segment;
(3) Guidewires with a tapered tip design, used to locate microchannels and/or possess certain puncturing capabilities, represented by Asahi’s Fielder XT series and Gaia series guidewires. Most CTO lesions can initially be attempted with this type of guidewire, and if unsuccessful, other types can be switched. This classification is not absolute; in practice, the characteristics of these guidewires overlap to a considerable extent, and operators typically choose guidewires based on the characteristics of the lesions and their own habits.
4
Selection of Guidewires
Correctly selecting a guidewire is one of the key factors for the success of interventional procedures. However, there are numerous guidewires produced by various manufacturers, each with different characteristics, and in fact, no operator can or needs to be familiar with all the characteristics of every guidewire. The characteristics of coronary lesions, the characteristics of guidewires, and the habits of the operator are the three main factors determining guidewire selection. Figure 4 summarizes commonly applicable guidewires in various situations for beginners’ reference.
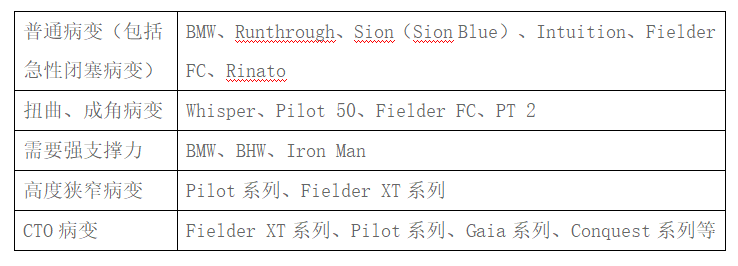
Figure 4
5
Guidewire Operational Techniques
Guidewire Shaping
Before inserting the guidewire, the operator should shape the tip based on the characteristics of the vascular lesions, the diameter of the vessel, the vessel’s configuration, and the angles between the main and branch vessels, typically shaping the tip into a “J” shape to facilitate the guidewire’s entry into curved or differently angled branch vessels. Shaping can be done using a wire guide or the shaping needle that comes with the guidewire, bending the guidewire’s distal end to a length approximately equal to or slightly smaller than the vessel’s diameter; for angles greater than 70° between the main and branch vessels, a second bend can be shaped about 1 cm from the first bend, making it easier for the guidewire to enter the larger angled branch vessels; for CTO lesions, the bend at the guidewire tip needs to be very small, generally around 1mm, with the Gaia series guidewires having a 1mm pre-shaped tip for beginners’ reference.
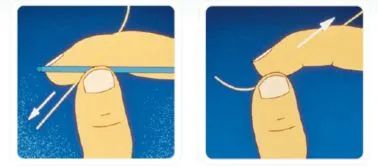
Figure 5 Guidewire Tip Shaping Diagram
Correctly Rotating and Pushing the Guidewire
When the guidewire reaches the catheter opening, inject a small amount of contrast agent to confirm that the catheter is at the coronary opening and coaxial, then slowly advance the guidewire into the coronary artery, rotating it slowly to moderately while gently pushing the guidewire, closely monitoring the guidewire tip. If resistance causes the guidewire tip to change shape, gently retract the guidewire, adjust the direction, and attempt to advance it again. During the guidewire insertion process, rotating the guidewire to align the tip’s direction with the vessel’s configuration is the most important part of guidewire operation. It is generally recommended to use a two-handed technique, with the left hand’s thumb and index finger gripping the guidewire to control its in-and-out distance, while the right hand’s thumb and index finger grip the knob (Torquer) to control the rotation speed and degree of the guidewire (Figure 6).
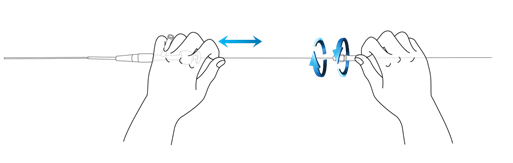
Figure 6 Guidewire Operation Diagram
A common issue to note is that all textbooks state: “Always push the guidewire without resistance“; however, many beginners misinterpret this statement, becoming hesitant in actual operations, making it difficult to smoothly advance the guidewire to the distal end of the lesion. Because the operator’s right hand’s rotation of the guidewire is difficult to completely synchronize with the guidewire tip, it is very challenging to rotate the guidewire tip to the appropriate, resistance-free direction. Maintaining a moderate speed of rotation at the guidewire tip is the most effective way to avoid resistance.
Therefore, an effective operational method is to maintain a moderate speed of rotation at the guidewire tip while gently advancing the guidewire, allowing the tip to automatically seek the direction of least resistance during rotation. However, it is crucial to note that once the guidewire tip encounters resistance and deforms, it needs to be retracted to restore the tip’s shape before attempting to advance it again.

Don’t want to missThe Voice of the Heart‘s updates?
Click the blue text at the top of the article“Heartream Voice of the Heart“ to follow us
And click the upper right corner “···” menu, select“Set as Favorite”