Dysphagia (噎膈, yē gé) is a condition characterized by difficulty swallowing due to dryness of the esophagus and narrowing of the esophagus and cardia, leading to food obstruction and, in severe cases, inability to swallow food into the stomach, with vomiting as the primary clinical manifestation. “Yē” refers to obstruction during swallowing, while “gé” indicates rejection, meaning that food cannot pass into the stomach, resulting in vomiting. The term “yē gé” encompasses both mild cases of dysphagia and can also be a precursor to more severe conditions, hence it is collectively referred to as dysphagia.
This condition typically occurs in older adults, particularly middle-aged and elderly men, and is currently considered difficult to treat. Therefore, if middle-aged and elderly individuals experience unexplained eating difficulties, they should seek medical attention promptly for relevant examinations to confirm the diagnosis and initiate early treatment.
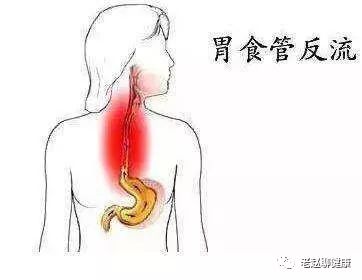
In Western medicine, conditions such as esophageal cancer, cardia cancer, esophagitis, cardia spasm, esophageal diverticulum, and diffuse esophageal spasm can present with symptoms of dysphagia. This section provides a reference for differential diagnosis and treatment.
The etiology of dysphagia primarily includes internal injuries from diet and emotions, aging with kidney deficiency, and dysfunction of the internal organs, with these factors often interrelated and mutually causative, leading to pathological changes characterized by deficiency and excess.
Initially, the condition is dominated by excess pathogenic factors, and as the disease progresses, qi stagnation, phlegm obstruction, and blood stasis become more pronounced, leading to increased narrowing of the esophagus and cardia. Additionally, due to the depletion of stomach fluids, kidney yin may be affected, resulting in deficiency of essence and blood, where the deficient state worsens. These two factors combine to form a severe case of dysphagia. In some patients, the condition may continue to progress, leading to yang deficiency due to yin damage, resulting in depletion of kidney essence and qi, and exhaustion of the spleen’s transformation function, ultimately leading to a critical state. The location of dysphagia is in the esophagus, which is governed by stomach qi and closely related to the liver, spleen, and kidneys.
The fundamental pathogenesis involves dysfunction of the spleen, stomach, liver, and kidneys, leading to dryness of fluids and blood, qi stagnation, phlegm obstruction, and blood stasis, resulting in dryness of the esophagus and narrowing of the esophagus and cardia.

Based on the pathogenesis of dysphagia, the treatment principles are to regulate qi and relieve stagnation, transform phlegm and eliminate stasis, nourish yin and blood, and moisten dryness, distinguishing between deficiency and excess. Initially, the focus is on treating excess, emphasizing the treatment of symptoms through regulating qi and relieving stagnation, transforming phlegm and eliminating stasis, with some support from nourishing yin and blood and moistening dryness; in later stages, the focus shifts to treating deficiency, or a combination of deficiency and excess, but the treatment emphasizes supporting the righteous qi, nourishing yin and blood, moistening dryness, or tonifying qi and warming yang, with some support from regulating qi and relieving stagnation, transforming phlegm and eliminating stasis. However, when treating symptoms, care should be taken to protect fluids and avoid excessive use of pungent, dispersing, and drying herbs; when treating the root, it is important to protect stomach qi and avoid excessive use of sweet and sour, cloying herbs. Maintaining even a small amount of fluids and stomach qi is of special significance in the differential diagnosis and treatment of dysphagia. Let’s take a look at the following:
Phlegm-Qi Obstruction
Symptoms: Food obstruction, fullness in the chest and diaphragm, and possibly pain; symptoms may improve with emotional relief and worsen with depression; belching, hiccups, vomiting phlegm and saliva, dry mouth and throat, difficult bowel movements, red tongue with thin greasy coating, and wiry slippery pulse.
Treatment method: Regulate stagnation and transform phlegm, moisten dryness and descend qi.
Formula: Qi Ge San (启膈散) modified.
Fluid Deficiency with Heat Accumulation
Symptoms: Painful obstruction during eating, fluids can be swallowed, but food is difficult to ingest, regurgitation after eating, burning pain in the chest and back, emaciation, dry skin, five hearts heat, dry mouth and throat, thirst for cold drinks, hard stools, red and dry tongue, possibly with cracks, and thin rapid pulse.
Treatment method: Nourish yin and generate fluids, clear heat and disperse accumulation.
Formula: Sha Shen Mai Dong Tang (沙参麦冬汤) modified.
Blood Stasis Internal Accumulation
Symptoms: Food obstruction, chest pain, inability to swallow food, even difficulty swallowing water, vomiting immediately after eating, dark complexion, dry skin, emaciation, hard stools resembling sheep droppings, or vomiting blood like red bean juice, or blood in stools, purple dark tongue, or red tongue with little fluid, and thin choppy pulse.
Treatment method: Break accumulation and move blood, nourish yin and blood.
Formula: Tong You Tang (通幽汤).
Qi Deficiency with Yang Weakness
Symptoms: Increasing obstruction during eating, inability to ingest food, pale complexion, fatigue, cold limbs, facial swelling, vomiting clear saliva, abdominal distension with loose stools, pale tongue with white coating, and thin weak pulse.
Treatment method: Warm and tonify spleen and kidneys, tonify qi and restore yang.
Formula: Warm Spleen and Tonify Qi Decoction (温脾用补气运脾汤) and Right Returning Pill (右归丸) modified.
Reflux
Symptoms: Fullness in the stomach after eating or vomiting before meals, morning food vomited in the evening, evening food vomited in the morning, undigested food, relief after vomiting, fatigue, pale complexion, cold hands and feet, loose stools, pale tongue, white slippery coating, and thin weak pulse. There is often a history of chronic stomach disease.
Treatment method: Warm the middle, strengthen the spleen, descend qi, and harmonize the stomach.
Formula: Ding Xiang Tou Ge San (丁香透膈散) modified.
In the stage of dysphagia where both the spleen and kidneys are failing, it is generally advisable to first use warming spleen and tonifying qi formulas to rescue the source of postnatal transformation. Once the patient can tolerate some food and medicine, then warming spleen and warming kidney formulas can be used, either in decoction or pill form, or alternating between the two. At this stage, if due to yang exhaustion above, food and fluids cannot enter, and yin exhaustion below leads to obstruction of urination and defecation, this is termed “guan ge” (关格), indicating a failure of the opening and closing mechanism, representing a separation of yin and yang, which requires active treatment. During this period, differential diagnosis is of utmost importance.

