Click “Shaanxi TCM” to subscribe!
Differentiation and Treatment of Internal Injury Fever

Internal injury fever refers to a condition caused by internal injury, characterized by dysfunction of the organs, stagnation of qi, blood, and dampness, or deficiency of qi, blood, yin, and yang, with fever as the main clinical manifestation. It generally has a slow onset and a prolonged course. Clinically, it often presents as low-grade fever, but can sometimes be high fever.
Qi Stagnation Fever
Symptoms: Fever is mostly low-grade or tidal, with fluctuations often corresponding to emotional changes, mental depression, fullness in the hypochondrium, irritability, dry and bitter mouth, reduced appetite, red tongue, yellow coating, and wiry rapid pulse.
Treatment Method: Soothe the liver, regulate qi, relieve depression, and clear heat.
Formula: Dan Zhi Xiao Yao San (Dan Zhi Free and Easy Wanderer Powder).
This formula soothes the liver and regulates the spleen, clearing liver heat. It includes Dan Pi (Moutan Cortex) and Zhi Zi (Gardenia) to clear liver heat, Chai Hu (Bupleurum) and Bo He (Mint) to soothe the liver and relieve heat, Dang Gui (Angelica) and Bai Shao (White Peony) to nourish blood and soften the liver, and Bai Zhu (Atractylodes) and Fu Ling (Poria) to tonify the spleen. If qi stagnation is severe, add Yu Jin (Curcuma) and Xiang Fu (Cyperus) to regulate qi and relieve depression; if heat symptoms are severe, with a red tongue and dry mouth, add Long Dan Cao (Gentiana) and Huang Qin (Scutellaria) to clear liver heat; for women with menstrual irregularities, add Ze Lan (Lycopus) and Yi Mu Cao (Leonurus) to invigorate blood and regulate menstruation.
Blood Stasis Fever
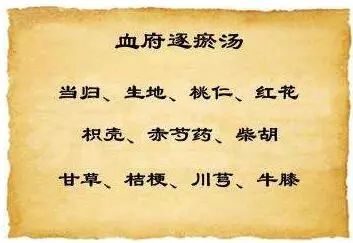
Symptoms: Fever in the afternoon or at night, or localized heat in certain body parts, dry throat with little desire to drink, fixed pain or swelling in limbs or body, pale or dark complexion, purple or stasis spots on the tongue, and wiry or choppy pulse.
Treatment Method: Invigorate blood and dispel stasis.
Formula: Xue Fu Zhu Yu Tang (Blood Mansion Drive Out Stasis Decoction).
This formula has good effects in invigorating blood and regulating qi, commonly used for blood stasis. It includes Dang Gui (Angelica), Chuan Xiong (Ligusticum), Chi Shao (Red Peony), and Di Huang (Rehmannia) to nourish and invigorate blood, Tao Ren (Peach Kernel), Hong Hua (Carthamus), and Niu Xi (Achyranthes) to invigorate blood and dispel stasis, Chai Hu (Bupleurum), Zhi Ke (Bitter Orange), and Jie Geng (Platycodon) to regulate qi and promote circulation, and Gan Cao (Licorice) to harmonize the herbs. If fever is severe, add Qin Jiao (Gentiana) and Bai Wei (Swertia) to clear heat and cool blood; for swelling and pain in limbs, add Dan Shen (Salvia), Yu Jin (Curcuma), and Yan Hu Suo (Corydalis) to invigorate blood and reduce swelling.
Damp Stagnation Fever

Symptoms: Low-grade fever, worse in the afternoon, chest tightness, epigastric fullness, heaviness throughout the body, lack of appetite, thirst without desire to drink, nausea, thin or sticky stools, white greasy or yellow greasy tongue coating, and slippery rapid pulse.
Treatment Method: Resolve dampness and clear heat.
Formula: San Ren Tang (Three Nut Decoction).
This formula has the effect of clearing damp-heat and promoting the flow of qi. It includes Xing Ren (Apricot Kernel) to descend lung qi, Sha Ren (Amomum) to transform dampness, Yi Yi Ren (Job’s Tears) to tonify the spleen and drain dampness, combined with Ban Xia (Pinellia) and Hou Po (Magnolia) to regulate qi and dry dampness; Tong Cao (Rice Paper Plant), Hua Shi (Talc), and Zhu Ye (Bamboo Leaf) to clear heat and resolve dampness, working together to promote the flow of qi and clear damp-heat.
If nausea is present, add Zhu Ru (Bamboo Shavings), Huo Xiang (Agastache), and Chen Pi (Tangerine Peel) to harmonize the stomach and descend counterflow; for chest tightness and greasy tongue coating, add Yu Jin (Curcuma) and Pei Lan (Eupatorium) to transform dampness; if damp-heat obstructs the Shaoyang, presenting with alternating chills and fever, with more heat than cold, and bitter mouth with nausea, add Qing Hao (Artemisia) and Huang Qin (Scutellaria) to clear and resolve Shaoyang.
Qi Deficiency Fever

Symptoms: Fever, either low or high, often occurring or worsening after exertion, fatigue, shortness of breath, spontaneous sweating, susceptibility to colds, reduced appetite, loose stools, pale tongue, thin white coating, and weak pulse.
Treatment Method: Tonify qi and strengthen the spleen, sweet and warm to clear heat.
Formula: Bu Zhong Yi Qi Tang (Tonify the Middle and Augment Qi Decoction).
This formula both tonifies qi and raises the sinking qi, representing a sweet and warm method to clear heat. It includes Huang Qi (Astragalus), Dang Shen (Codonopsis), Bai Zhu (Atractylodes), and Gan Cao (Licorice) to tonify qi and strengthen the spleen; Dang Gui (Angelica) to nourish and invigorate blood; Chen Pi (Tangerine Peel) to regulate qi and harmonize the stomach; Sheng Ma (Cimicifuga) and Chai Hu (Bupleurum) to both lift clear yang and release heat evil.
If spontaneous sweating is excessive, add Mu Li (Oyster Shell), Fu Xiao Mai (Wheat), and Nuo Mi Gen (Glutinous Rice Root) to stabilize the exterior and restrain sweating; for alternating chills and fever with sweating and aversion to wind, add Gui Zhi (Cinnamon Twig) and Bai Shao (White Peony) to harmonize the nutritive and defensive qi; if spleen deficiency with dampness presents as chest tightness and epigastric fullness, with a white greasy tongue coating, add Cang Zhu (Atractylodes) and Fu Ling (Poria) to strengthen the spleen and dry dampness.
Blood Deficiency Fever
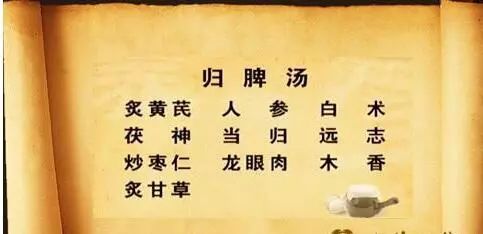
Symptoms: Fever, mostly low-grade, dizziness, fatigue, palpitations, pale complexion, pale lips and nails, pale tongue, and weak pulse.
Treatment Method: Tonify qi and nourish blood.
Formula: Gui Pi Tang (Restore the Spleen Decoction).
This formula tonifies the heart and spleen, benefiting qi and generating blood, commonly used for blood deficiency. It includes Huang Qi (Astragalus), Dang Shen (Codonopsis), Fu Ling (Poria), Bai Zhu (Atractylodes), and Gan Cao (Licorice) to tonify qi and strengthen the spleen, Dang Gui (Angelica) and Long Yan Rou (Longan) to nourish and invigorate blood; Suan Zao Ren (Sour Jujube Seed) and Yuan Zhi (Polygala) to nourish the heart and calm the spirit; Mu Xiang (Aucklandia) to strengthen the spleen and regulate qi, ensuring the formula tonifies without stagnation.
If blood deficiency is severe, add Shu Di Huang (Rehmannia), Gou Qi Zi (Goji Berry), and Zhi He Shou Wu (Processed Fo-Ti) to nourish essence and blood; if fever is severe, add Yin Chai Hu (Lonicera) and Bai Wei (Swertia) to clear and eliminate empty heat; for blood deficiency due to chronic bleeding, if there is still slight bleeding, consider adding San Qi Powder, Xian He Cao (Agrimonia), Qian Cao (Rubia), and Palm Bark to stop bleeding.
Yin Deficiency Fever
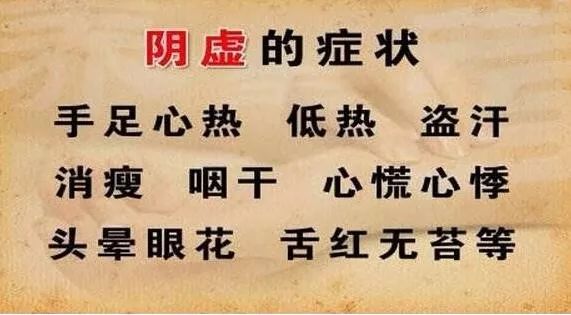
Symptoms: Tidal fever in the afternoon or night, aversion to clothing, hot palms and soles, irritability, insomnia with many dreams, night sweats, dry mouth and throat, red tongue, or cracks, little or no coating, and thin rapid pulse.
Treatment Method: Nourish yin and clear heat.
Formula: Qing Gu San (Clear the Bones Powder).
This formula has the effect of nourishing yin and clearing heat, reducing fever and eliminating steaming. It includes Yin Chai Hu (Lonicera), Zhi Mu (Anemarrhena), Hu Huang Lian (Coptis), Di Gu Pi (Lycium), Qing Hao (Artemisia), and Qin Jiao (Gentiana) to clear empty heat, Bie Jia (Soft-Shelled Turtle) to nourish yin and subdue yang, and Gan Cao (Licorice) to harmonize the herbs. If night sweats are severe, remove Qing Hao and add Mu Li (Oyster Shell), Fu Xiao Mai (Wheat), and Nuo Mi Gen (Glutinous Rice Root) to stabilize the exterior and restrain sweating; if yin deficiency is severe, add Xuan Shen (Scrophularia), Sheng Di (Rehmannia), and Zhi He Shou Wu (Processed Fo-Ti) to nourish yin essence; for insomnia, add Suan Zao Ren (Sour Jujube Seed), Bai Zi Ren (Platycladus), and Ye Jiao Teng (Polygala) to nourish the heart and calm the spirit; if there is qi deficiency with dizziness, shortness of breath, and fatigue, add Bei Sha Shen (Glehnia), Mai Dong (Ophiopogon), and Wu Wei Zi (Schisandra) to tonify qi and nourish yin.
Yang Deficiency Fever

Symptoms: Fever with a desire for warmth, feeling cold, cold limbs, shortness of breath, lethargy, dizziness, weakness in the lower back and knees, reduced appetite, loose stools, pale complexion, pale tongue, or teeth marks, white moist coating, and deep thin pulse.
Treatment Method: Warm and tonify yang qi, guiding fire back to the source.
Formula: Jin Gui Shen Qi Wan (Kidney Qi Pill from the Golden Cabinet).
This formula is commonly used to warm and tonify kidney yin, although it is a warming yang formula, it also includes herbs that nourish yin, signifying the balance of yin and yang. As stated in the “Jing Yue Quan Shu: New Formulas Overview”, “To effectively tonify yang, one must seek yang within yin, allowing yang to be supported by yin for boundless transformation.” The formula includes Fu Zi (Aconite) and Rou Gui (Cinnamon) to warm and tonify yang qi, Shan Zhu Yu (Cornus) and Di Huang (Rehmannia) to nourish the liver and kidneys, Shan Yao (Chinese Yam) and Fu Ling (Poria) to tonify the kidneys and strengthen the spleen, and Dan Pi (Moutan Cortex) and Ze Xie (Alisma) to clear and drain the liver and kidneys as assistants. For severe shortness of breath, add Ren Shen (Ginseng) to tonify original qi; for loose stools and diarrhea, add Bai Zhu (Atractylodes) and Pao Gan Jiang (Dried Ginger) to warm and transport the middle jiao.
Expert Introduction:
Zeng Shenghai: Male, Chief Physician at Baoji TCM Hospital, First Renowned TCM Physician in Shaanxi Province, First Renowned TCM Physician in Baoji City, Master’s Supervisor, National Fourth Batch, Provincial Second Batch, Fourth Batch, Fifth Batch Renowned Old TCM Academic Experience Inheritance Guidance Teacher, Doctoral Professional Degree Mentor at the Clinical Medicine (TCM Inheritance) of the Chinese Academy of Traditional Chinese Medicine, Part-time Professor of TCM Internal Medicine at Shaanxi University of Traditional Chinese Medicine, and a member of the National Association of Integrated Traditional Chinese and Western Medicine Digestive Diseases, and a council member of the Shaanxi Association of Traditional Chinese Medicine.
(Source: Baoji TCM Hospital, Zeng Shenghai)
This issue coordinated by: Kong Qun
This issue reviewed by: Zhao Wen
This issue edited by: Wang Shuangpei
Public Account ID: snatcm
Official WeChat of Shaanxi Provincial Administration of Traditional Chinese Medicine
■ Please click the blue font “Shaanxi TCM” at the bottom right of the title or long press the QR code on the right to follow us.

■ Reprinting is welcome, please indicate the source! ■ Contributions are welcome at [email protected]
■ This article is the 512th issue of “Shaanxi TCM”.