Ye Tianshi’s Gynecological Case Study Notes: Three Methods for Regulating Menstruation and Balanced Supplementation

Case 1: Gu, with menstrual cramps and abdominal pain, often experiences heart pain and dry vomiting. This is due to liver qi stagnation, affecting the Chong and Ren meridians. The focus is on promoting the flow of qi and blood to regulate menstruation, avoiding warming and drying methods, which can yield results.
Chuan Lian Zi (Fructus Meliae) 1 qian, Dan Pi (Moutan Cortex) 3 qian, Chao Zha (Fructus Crataegi) 2 qian, Hu Lian (Rhizoma Coptidis) 8 fen, Yan Hu Suo (Rhizoma Corydalis) 1 qian, Ze Lan (Herba Lycopi) 2 qian, Gui Xu (Radix Rehmanniae) 2 qian, Sheng Bai Shao (Radix Paeoniae) 1.5 qian
Also, Bai Zi Ren Wan (Semen Platycladi Pill).
Case 2: Wu, with qi stagnation affecting the meridians, experiences dysmenorrhea.
Chuan Xiong (Rhizoma Chuanxiong), Dang Gui (Radix Angelicae Sinensis), Xiang Fu (Rhizoma Cyperi), Xiao Hui Xiang (Fructus Foeniculi), Wu Yao (Rhizoma Linderae), Fu Ling (Poria), Hong Zao (Fructus Jujubae)
Case 3: Fei, with dark purple menstrual blood, experiences noisy menstruation, with a pulse that is tight and painful, accompanied by continuous leukorrhea, weight loss, and a pulse that is strong on the right and weak on the left. The upper body is hot, while the lower body is cold to the bone, indicating a disharmony of yin and yang, making conception difficult. All physicians suggest using blood tonics, which may yield little effect. The method of promoting yang and nourishing yin is recommended.
Abalone (Haliotis), Sheng Di (Radix Rehmanniae), Dan Cong (Herba Cistanches), Tian Dong (Asparagus), Dang Gui (Radix Angelicae Sinensis), Bai Zi Ren (Semen Platycladi), Chao Shan Zha (Fructus Crataegi), Niu Xi (Radix Achyranthis) and Fu Ling (Poria)
Hong Zao and Qi Ai Decoction Pills.

1. Case Analysis and Differentiation of Patterns
Gu’s Case: Liver Qi Stagnation, Disharmony of Chong and Ren
– Main Symptoms: Menstrual cramps, abdominal pain, heart pain, and dry vomiting.
– Pathogenesis: Liver qi rising, obstructing the Chong and Ren, leading to qi and blood stagnation, which over time transforms into heat.
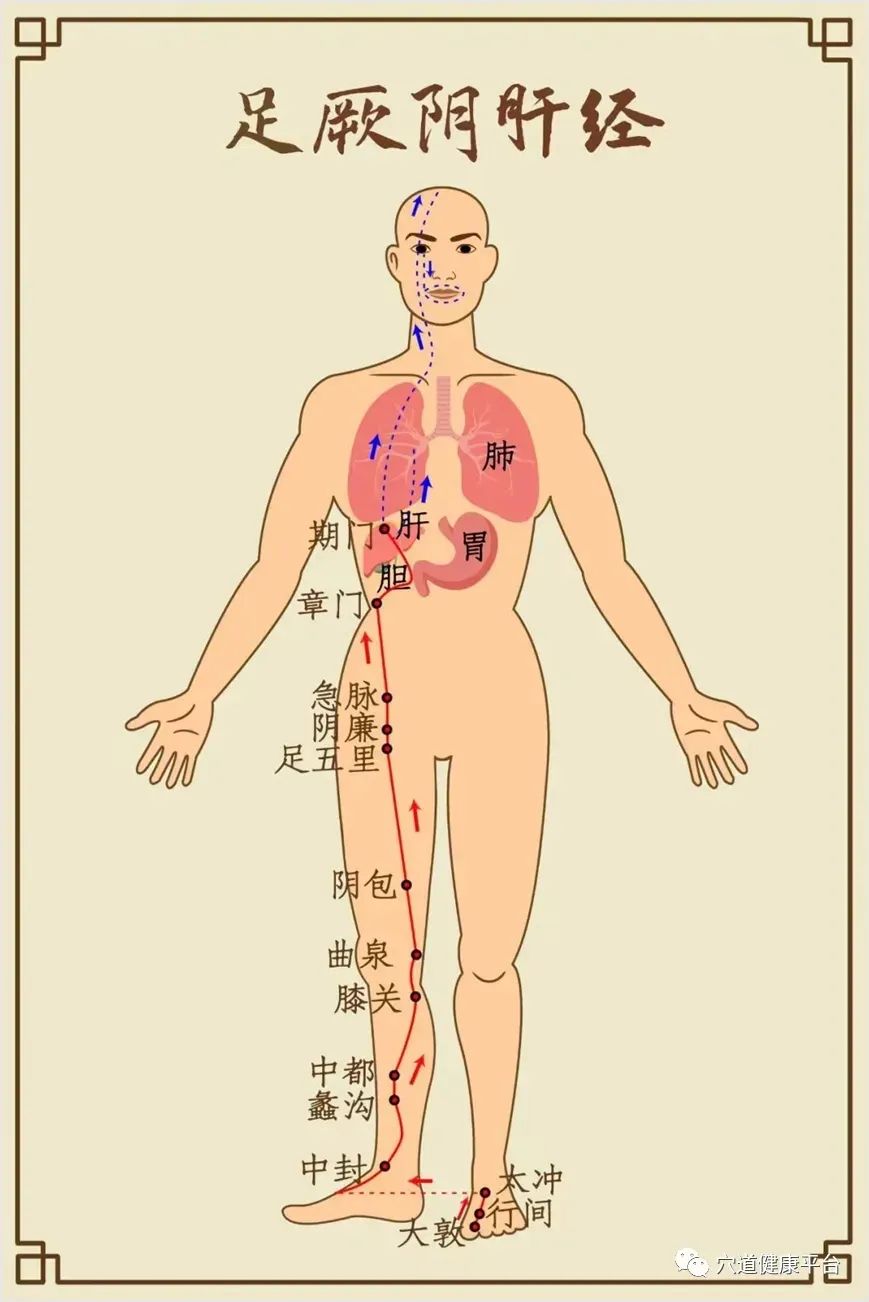
– Liver qi stagnation: The liver meridian runs through the lower abdomen, disturbing the chest diaphragm, hence the abdominal pain, heart pain, and dry vomiting;
According to the Ling Shu: Meridians:The liver meridian of the foot Jueyin begins at the junction of the big toe, ascends along the foot, goes one cun above the inner ankle, eight cun above the ankle, crosses the Taiyin, ascends along the inner thigh, enters the pubic area, connects with the stomach, belongs to the liver and gallbladder, ascends through the diaphragm, spreads to the ribs, runs behind the throat, ascends to the temples, connects with the eyes, exits at the forehead, and meets the Du meridian at the crown; its branches run from the eyes down to the cheeks, encircling the lips; another branch runs from the liver, crosses the diaphragm, and enters the lungs.
– Disharmony of Chong and Ren: Qi and blood stagnation leads to obstructed menstruation and lack of nourishment to the meridians, resulting in pain.
– Treatment Method: Clear the liver, descend the qi, invigorate blood, and avoid warming and drying methods.
– Medications:
– Chuan Lian Zi, Hu Huang Lian: Clear the liver, drain heat, descend qi, and stop vomiting;
– Dan Pi, Chi Shao (Gui Xu, Bai Shao): Cool blood, soften the liver, harmonize the nutrients, and relieve pain;
– Yan Hu Suo, Ze Lan, Chao Shan Zha: Invigorate blood, regulate menstruation, and resolve stagnation;
– Bai Zi Ren Wan: Nourish the heart, calm the spirit, moisten dryness, and open the meridians (to prevent prolonged stagnation from injuring yin).
Wu’s Case: Qi Stagnation and Blood Stasis, Pain During Menstruation
– Main Symptoms: Dysmenorrhea, accompanied by symptoms of qi stagnation in the meridians.
– Pathogenesis: Emotional stagnation, qi stagnation, and blood stasis, leading to obstruction of the meridians.
– Qi stagnation is primary: The liver fails to disperse, leading to poor qi flow;
– Stasis is the result: Qi and blood stagnation cause abdominal pain during menstruation.
– Treatment Method: Soothe the liver, regulate qi, invigorate blood, and strengthen the spleen and harmonize the center.
– Medications:
– Chuan Xiong, Xiang Fu, Wu Yao: Soothe the liver, move qi, regulate menstruation, and relieve pain;
– Dang Gui, Xiao Hui Xiang: Invigorate blood, warm the channels, disperse cold, and resolve stasis;
– Fu Ling, Hong Zao: Strengthen the spleen, benefit qi, and prevent the qi-regulating herbs from injuring the middle jiao.
Fei’s Case: Disharmony of Yin and Yang, Heat Above and Cold Below
– Main Symptoms: Dark purple menstrual blood, clear and thin leukorrhea, weight loss, heat above (rising fire) and cold below (cold penetrating to the bone).
– Pathogenesis: Disharmony of yin and yang, deficiency of the Chong and Ren, with deficiency of the upper jiao’s fire and cold in the lower jiao.
– Yin blood deficiency: Dark purple menstrual blood, weight loss, and a weak left pulse;
– Yang deficiency with cold stagnation: Cold pain in the lower jiao, clear and thin leukorrhea, and a strong right pulse (floating and weak yang).
– Treatment Method: Promote yang and nourish yin, harmonize the Chong and Ren, and connect the heart and kidney.
– Medications:
– Abalone, Sheng Di, Tian Dong: Nourish yin, replenish essence, and clear the floating fire in the upper jiao;
– Cistanches, Qi Ai: Warm the kidney, warm the uterus, and disperse cold stagnation in the lower jiao;
– Dang Gui, Bai Zi Ren, Niu Xi: Nourish blood, calm the spirit, and guide blood downward;
– Shan Zha, Fu Ling: Strengthen the spleen, resolve accumulation, and prevent dampness from obstructing the stomach.
2. Insights on Medication
Clear the liver and drain heat, avoid using harsh methods
– For liver qi stagnation transforming into fire (as in Gu’s case), use Chuan Lian Zi and Hu Huang Lian to clear the liver, paired with Bai Shao to soften the liver, avoiding Chai Hu, Gui Zhi, and other warming herbs that assist fire.
– Modern Application: For menopausal syndrome with hot flashes and irritability, add Xia Ku Cao and Bai Wei to enhance the clearing effect.
Soothe the liver and regulate qi, while considering the spleen and stomach
– For qi stagnation and blood stasis (as in Wu’s case), use Xiang Fu and Wu Yao to move qi, supplemented with Fu Ling and Hong Zao to strengthen the spleen, reflecting the idea of “treating the liver while supporting the spleen.”
– Modern Application: For primary dysmenorrhea, add rose and monthly flower to soothe the liver, combined with Shan Yao and Lian Zi to protect the middle jiao.
Promote yang and nourish yin, using both cold and heat
– For both yin and yang deficiency (as in Fei’s case), use Abalone and Sheng Di to nourish yin, while Cistanches and Ai Ye warm yang, balancing cold and heat to restore harmony in the Chong and Ren.
– Modern Application: For ovarian dysfunction with cold in the uterus leading to infertility, this formula can be adapted by adding Zi He Che and Lu Jiao Shuang to replenish the extraordinary meridians.
Invigorate blood and resolve stasis, selecting medications based on the meridian
– For abdominal pain in the lower abdomen (Jueyin meridian), use Ze Lan and Yan Hu Suo;
– If accompanied by leukorrhea (Ren meridian), use Niu Xi and Fu Ling to guide the medication downward.
3. Insights on Differentiation
Emphasize the core role of liver qi in gynecological diseases
– All three cases involve liver stagnation, but the treatment methods differ:
– Gu’s case focuses on clearing and descending liver qi;
– Wu’s case emphasizes soothing and dispersing liver qi;
– Fei’s case requires nourishing yin and blood due to deficiency.
The Chong and Ren are the sea of qi and blood; regulating menstruation must solidify the extraordinary meridians
– Gu’s case shows that the Chong and Ren are affected by liver qi stagnation, requiring descending and opening the meridians;
– Fei’s case indicates deficiency in the Chong and Ren, with both yin and yang deficient, necessitating both promotion and supplementation.
Pulse and symptoms should be correlated to distinguish deficiency and excess
– Gu’s case has an unclear pulse, but the note “avoid warming and drying” suggests a tendency towards heat;
– Fei’s case shows a strong right pulse and weak left pulse, indicating excess above and deficiency below;
– Wu’s case is primarily characterized by pain, and the pulse should be tight and rough, indicating qi stagnation and excess.
Dynamic observation and stepwise treatment
– Gu’s case first uses decoctions for urgent treatment (clearing the liver and invigorating blood), followed by Bai Zi Ren Wan for gradual treatment (nourishing the heart and calming the spirit);
– Fei’s case uses pills for gradual treatment, considering the spleen and stomach’s function.
4. Learning Insights and Clinical Expansion
Expanding from “liver qi stagnation” to modern diseases
– Application Scenario: For dysmenorrhea associated with endometriosis and gastrointestinal symptoms (such as nausea and diarrhea), refer to Gu’s case approach, using Chuan Lian Zi and Yan Hu Suo combined with Shao Yao Gan Cao Decoction for urgent pain relief.
Application of the “promoting yang and nourishing yin” method in reproductive endocrine diseases
– For premature ovarian failure: adapt Fei’s case using Gui Jia, Cistanches, and Zi Shi Ying to replenish yin and yang, combined with acupuncture to nourish the Ren and Du meridians.
Meridian disease theory guiding chronic gynecological diseases
– For chronic pelvic inflammatory disease: prolonged illness enters the meridians, using Ze Lan and Dan Shen to resolve stasis and open the meridians, supplemented with Hong Teng and Bai Jiang Cao to clear heat.
Focus on emotional and physical regulation
– Patients with liver qi stagnation (like Wu’s case) need psychological counseling, and can drink jasmine tea daily to soothe the liver and relieve depression;
– Those with both yin and yang deficiency (like Fei’s case) should avoid staying up late, and dietary therapy can include Ejiao stewed with black chicken to nourish yin and warm yang.
5. Conclusion
Although Ye Tianshi’s three cases all fall under the category of gynecological dysmenorrhea, the treatment methods differ significantly due to variations in pathogenesis, fully reflecting the essence of “same disease, different treatment” in differentiation. The medications used are light and precise, such as using Chuan Lian Zi to clear the liver, Bai Zi Ren to moisten dryness, and Abalone to nourish yin, all demonstrating ingenuity. Modern clinical practice should learn from these methods:
– Focus on the liver as the foundation, prioritizing the smooth flow of qi;
– Use the extraordinary meridians as the root, balancing promotion and supplementation of yin and yang;
– Use pulse and symptoms as the basis, dynamically adjusting strategies.
Only then can we unravel the complexities of gynecological diseases, achieving effective results.

