The editor updates the key content of the chapter on Traditional Chinese Medicine (TCM) pharmacy shared by enthusiastic member I Can Do It, along with an analysis of the 2013 exam questions. Everyone is welcome to learn together!
If you find it helpful, please click the lower left corner to read the original text and reply to support the student who organized and shared this!
If you cannot reply, you can return to WeChat, send “bind” to the TCM circle for registration or binding, and then you can reply to support. The end of the article contains the exam questions from 2013 for this chapter!
The key content in the original text will be more prominent
1. Characteristics and Classification of External Preparations
1.1 Characteristics of the Administration System: The medication penetrates the skin into the systemic circulation, avoiding the first-pass effect in the liver, preventing destruction in the gastrointestinal tract, reducing peak and trough variations in blood drug concentration, and lowering side effects of the medication.
1.2 Classification: Ointments, plasters (black and white), adhesive patches (rubber patches, gel patches, adhesive dressings)
2. Pathways and Influencing Factors of Transdermal Drug Absorption
2.1 Process of Transdermal Absorption: Release → Penetration → Absorption
2.2 Pathways of Transdermal Absorption: Intact epidermis – the main pathway
2.3 Factors Influencing Transdermal Absorption (X-type questions)
(1) Skin Conditions
① Application Site
② Skin Lesions
③ Skin Temperature and Humidity
④ Skin Cleanliness
(2) Drug Properties
Ideal drugs: have suitable oil-water partition coefficients, possessing both lipophilicity and hydrophilicity
(3) Composition and Properties of the Matrix
① Composition, type, and properties of the matrix; different matrices for ointment absorption: emulsion-type matrix > hydrophilic ointment matrix (Vaseline + lanolin), silicone, lard > hydrocarbon water-soluble matrix; polyethylene glycol releases drugs quickly but has little effect on drug penetration, making the resulting ointment difficult to absorb transdermally.
② pH of the matrix < weak acid drug pKa or > weak base drug pKa, significantly increases the molecular form of the drug, facilitating absorption.
③ Additives: Surfactants, transdermal penetration enhancers
④ Matrices that increase skin hydration can also enhance drug permeability; matrices with strong oiliness have strong occlusiveness, significantly increasing skin hydration.
(4) Other Factors: Drug concentration, application area, frequency of application, and contact time with the skin are closely related.
3. Matrix of Ointments
3.1 Oleaginous Matrix
1. Characteristics
Advantages:
① Lubricating, non-irritating;
② Can occlude the skin surface, promoting skin hydration, providing better protection and softening effects than other matrices;
③ Compatible with various drugs
Disadvantages:
① Greasy and hydrophobic;
② Poor drug release;
③ Difficult to mix with aqueous liquids;
④ Not easily washed off with water;
⑤ Not suitable for acute inflammatory exudative wounds.
3.2 Classification and Representative Varieties
① Hydrocarbons: Vaseline
② Lipid types: Lanolin, beeswax, white wax, whale wax.
③ Oils: Animal oils, vegetable oils (peanut oil, sesame oil), hydrogenated vegetable oils.
④ Silicone types: Silicones, but irritating to the eyes, not suitable as an eye ointment matrix.
3.3 Emulsion-type Matrix
1. Characteristics
① Has certain affinity for both oil and water, facilitating drug release and penetration;
② Can absorb exudates from wounds, easy to apply and wash off;
③ Can be used for subacute, chronic, non-exudative skin diseases, contraindicated for erosive, ulcerative, and purulent wounds;
④ Water-unstable drugs should not be made into emulsion-type ointments.
2. Classification and Representative Varieties – Oil-in-water type, water-in-oil type
3.4 Water-soluble Matrix
Characteristics:
① Fast drug release;
② No greasiness or irritation;
③ Can absorb tissue exudates, suitable for erosive wounds and mucous membranes;
④ Poor lubricating effect;
⑤ Prone to dehydration and mold, thus requiring the addition of moisturizers and preservatives.
Classification and Representative Varieties:
1. Cellulose derivatives: Methylcellulose, sodium carboxymethylcellulose, etc.
2. Polyethylene glycol (PEG) mixed with benzoic acid, tannic acid, phenol can excessively soften the matrix, reducing the preservative ability of phenolic preservatives; long-term use can lead to skin dryness.
3. Carbomer: Especially suitable for the treatment of seborrheic dermatitis.
4. Others: Sodium alginate, glycerin gelatin.
4. Preparation of Ointments
1. Methods of Adding Drugs
(1) Co-melting components are ground and mixed with the matrix at around 40°C.
(2) Volatile or heat-sensitive drugs
2. Preparation Methods (Applicable Drugs)
(1) Grinding method
(2) Melting method (hot melting method)
(3) Emulsification method
5. Eye Ointments – Sterile Preparations
1. Definition: Eye ointments refer to sterile ointments made from drugs and suitable matrices for ophthalmic use. Commonly used matrix – Vaseline: Liquid paraffin: Lanolin = 8:1:12. Preparation Key Points: Aseptic operation, matrix: dry heat sterilization at 150°C for 1-2 hours.
3. Quality Requirements
(1) Eye ointments should be uniform, fine, non-irritating to the eyes, and easy to apply to the eyes, facilitating drug dispersion and absorption.
(2) The matrix should be filtered and sterilized before preparation.
(3) Unless otherwise specified, the amount in each container should not exceed 5g.
(4) Suspended eye ointments must not contain particles larger than 90μm.
(5) Metal foreign body inspection.
6. Black Plasters
1. Raw Materials for the Matrix
(1) Plant oils: Sesame oil (best), cottonseed oil, soybean oil, rapeseed oil, peanut oil.
(2) Red lead: A reddish-orange non-crystalline powder, its main component is lead tetroxide (Pb3O4), with a content requirement of over 95%.
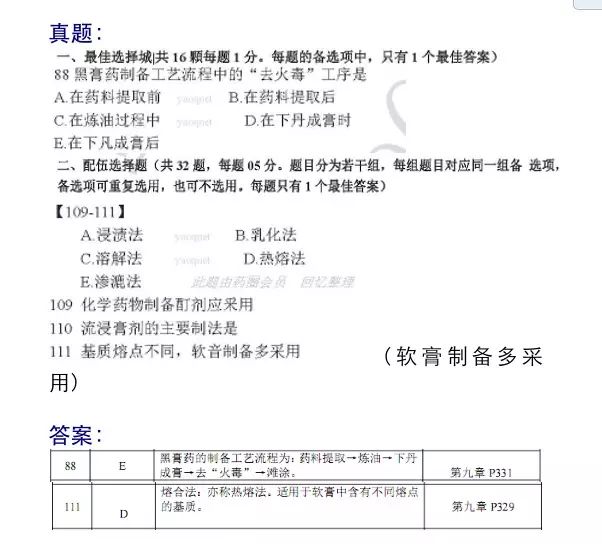
2. Preparation Process of Black Plasters: Extraction of medicinal materials (frying) → Refining oil → Adding lead to form paste → Removing “fire toxins” → Spreading.
7. Rubber Plasters
1. Composition of Rubber Plaster Matrix (B-type questions)
(1) Rubber: Main matrix
(2) Adhesives: Increase the viscosity of the paste, glycerin rosin ester, hydrogenated rosin, β-pinene
(3) Softening agents: Common softening agents: Vaseline, lanolin, liquid paraffin, vegetable oils, dibutyl phthalate, dioctyl phthalate.
(4) Fillers: Zinc oxide (pharmaceutical grade), zinc barium white (commonly known as Lide powder). Zinc oxide as a filler can form zinc salts with rosin acid, increasing the adhesion of the paste to the backing material; it can also reduce the irritation of rosin acid to the skin, having a mild astringent effect. When making rubber plasters by hot pressing, zinc barium white is commonly used as a filler, characterized by strong coverage and high hardness of the paste.
(5) Solvents: Dissolve the matrix, gasoline, n-hexane, which need to be recovered and removed.
2. Preparation Methods for Rubber Plasters
① Solvent method (commonly used) Process: Extraction of medicinal materials → Preparation of paste → Coating → Recovery of solvent → Cutting → Lining → Packaging.
② Hot pressing method
8. Gel Plasters (Babu Plasters) Hydrophilic Matrix
1. Characteristics: Convenient to use, comfortable to apply, non-irritating to the skin. The matrix is hydrophilic, facilitating transdermal absorption of drugs.
2. Composition of Gel Plasters
Backing materials: Bleached cloth, non-woven fabric protective layer (covering material for the paste): Polyethylene film paste layer: Drug + matrix (sodium polyacrylate, sodium carboxymethylcellulose, gelatin, glycerin, and micro-powdered silica)